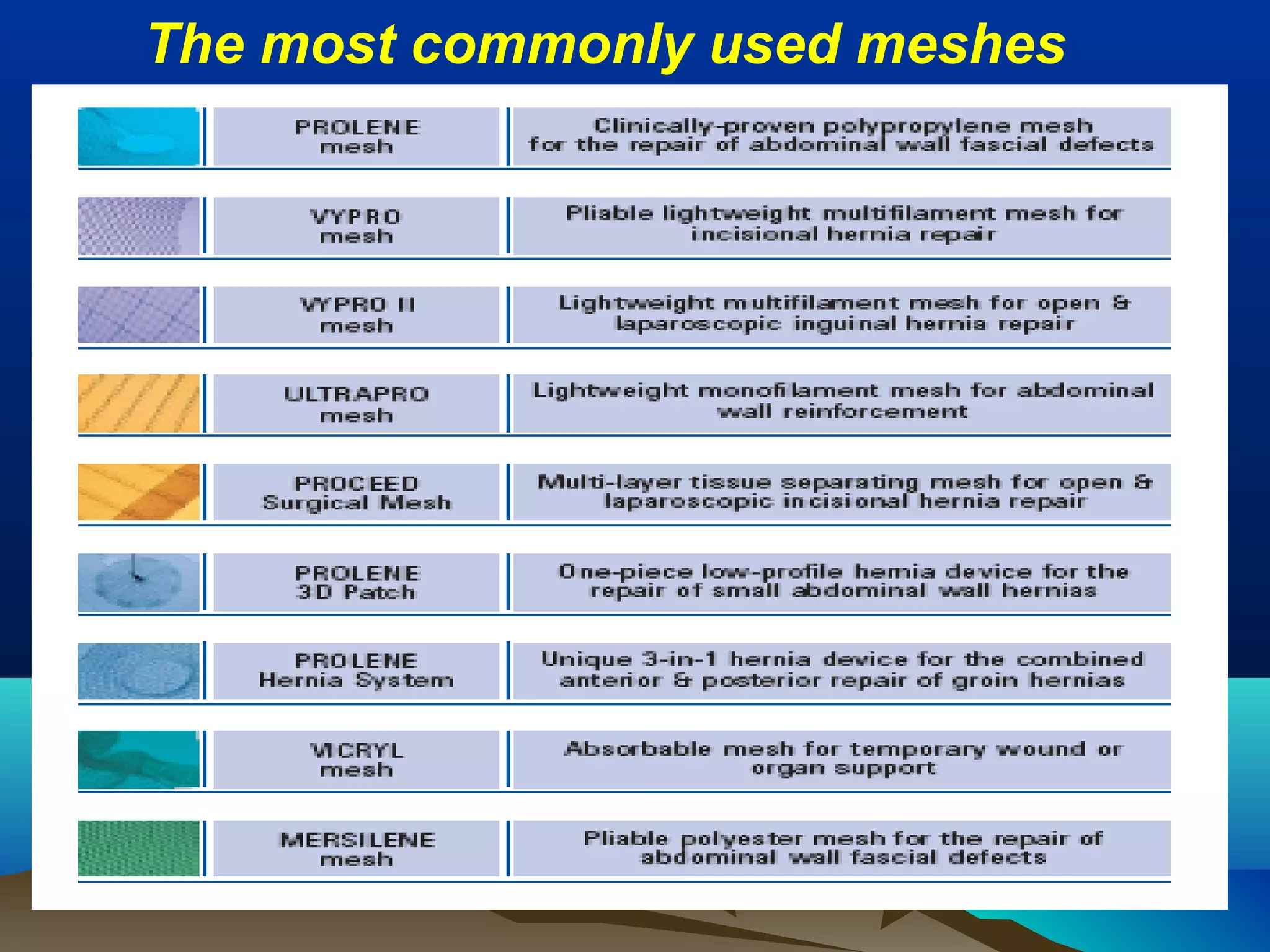
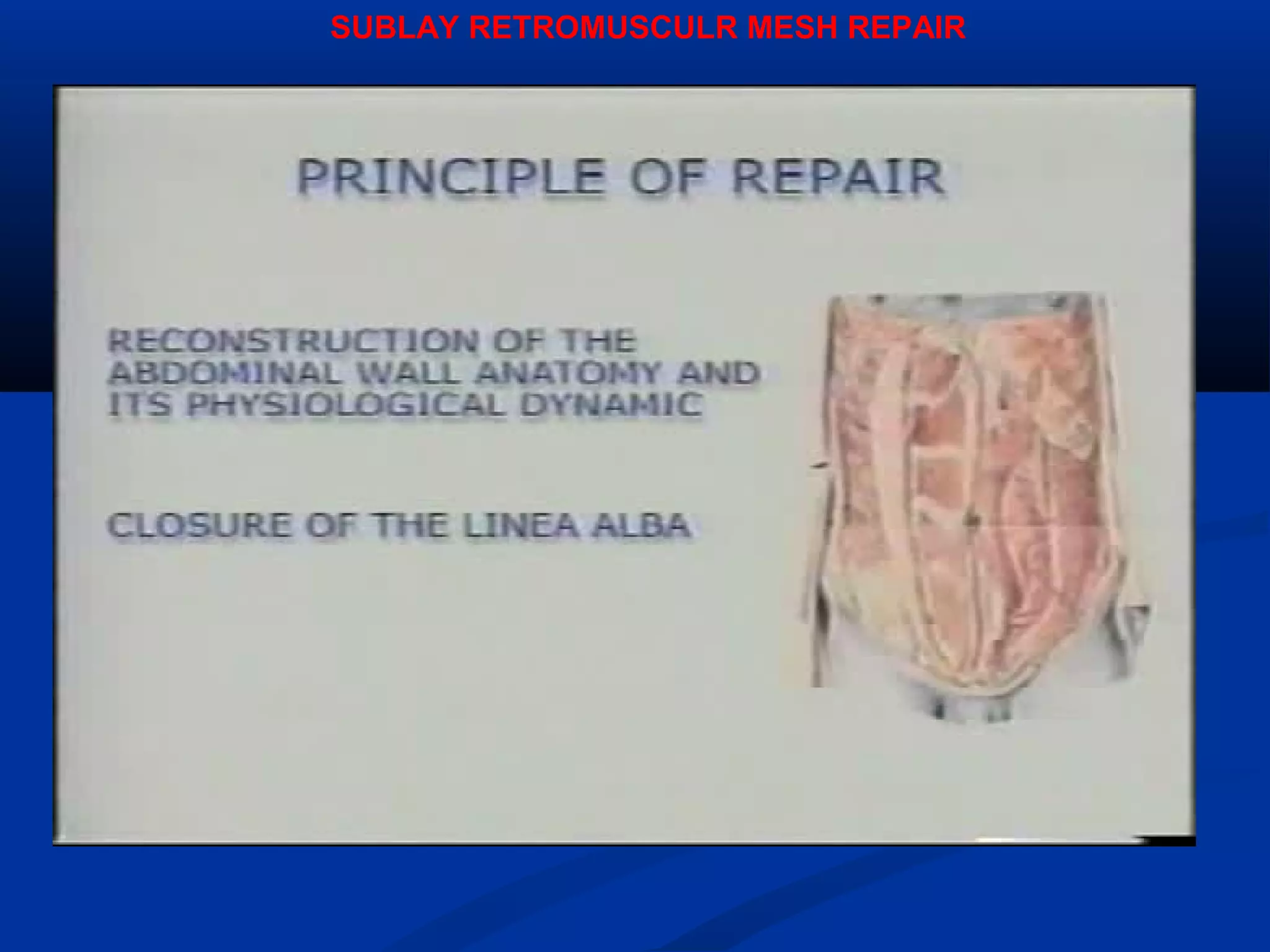
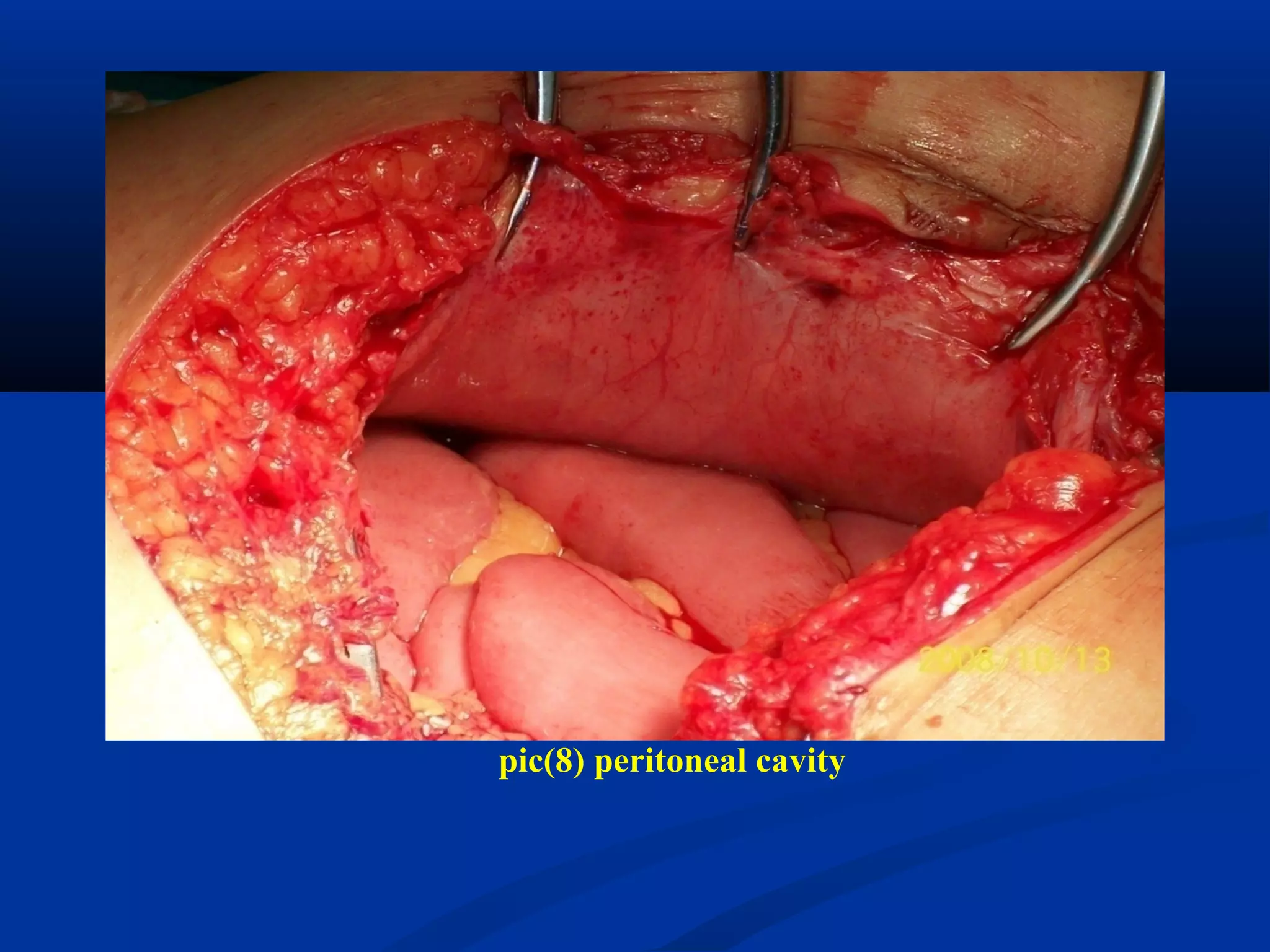
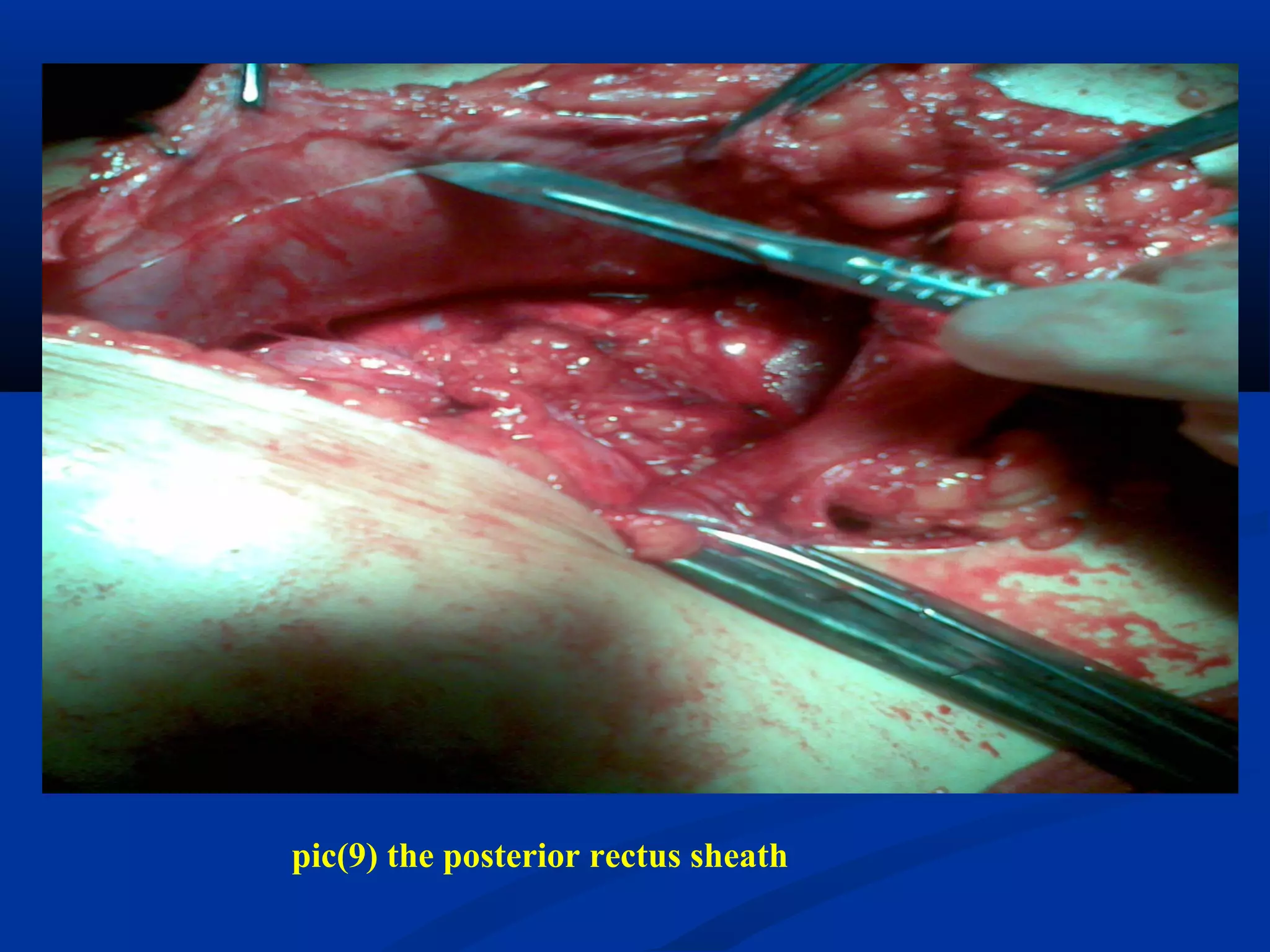
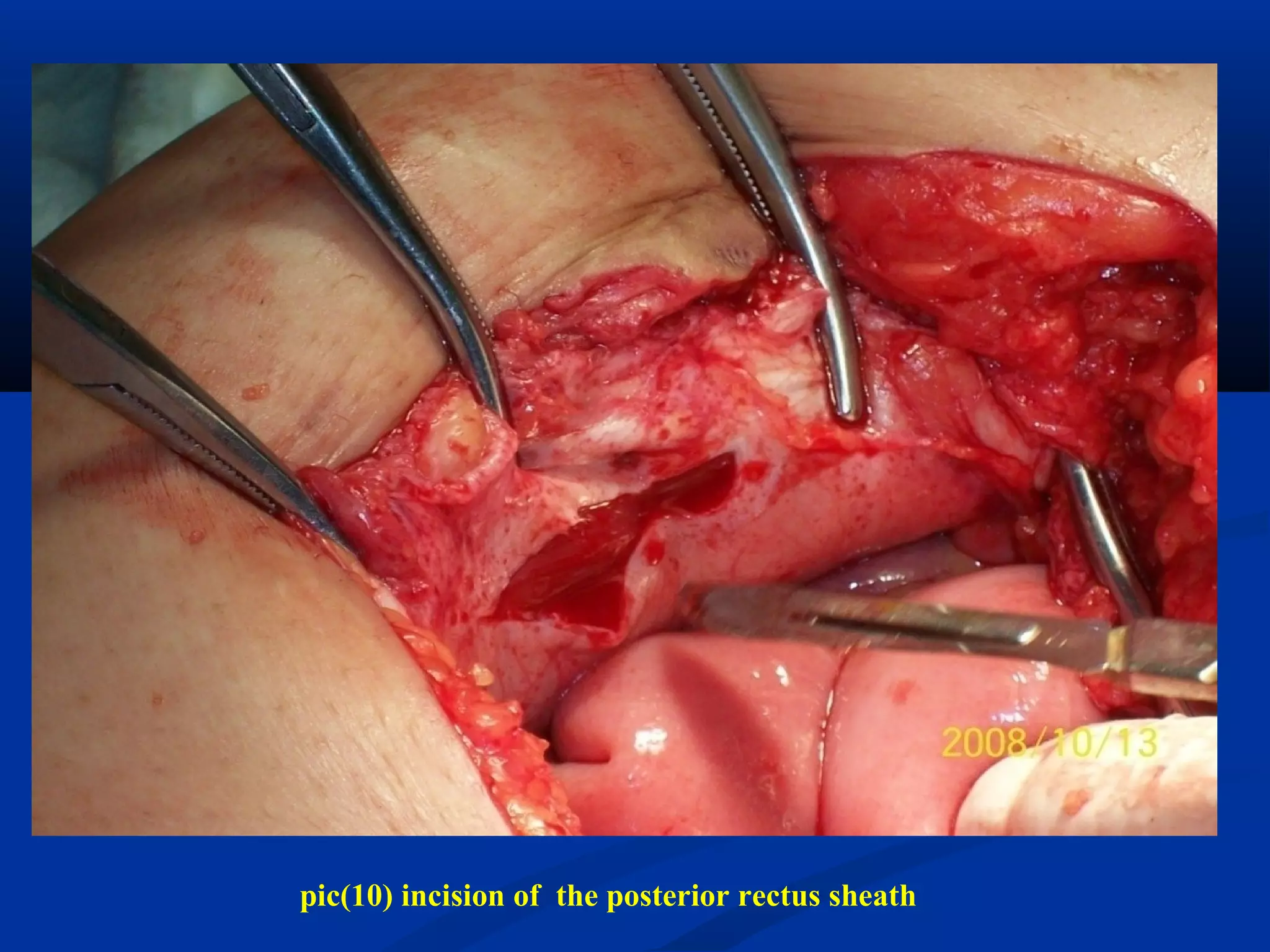
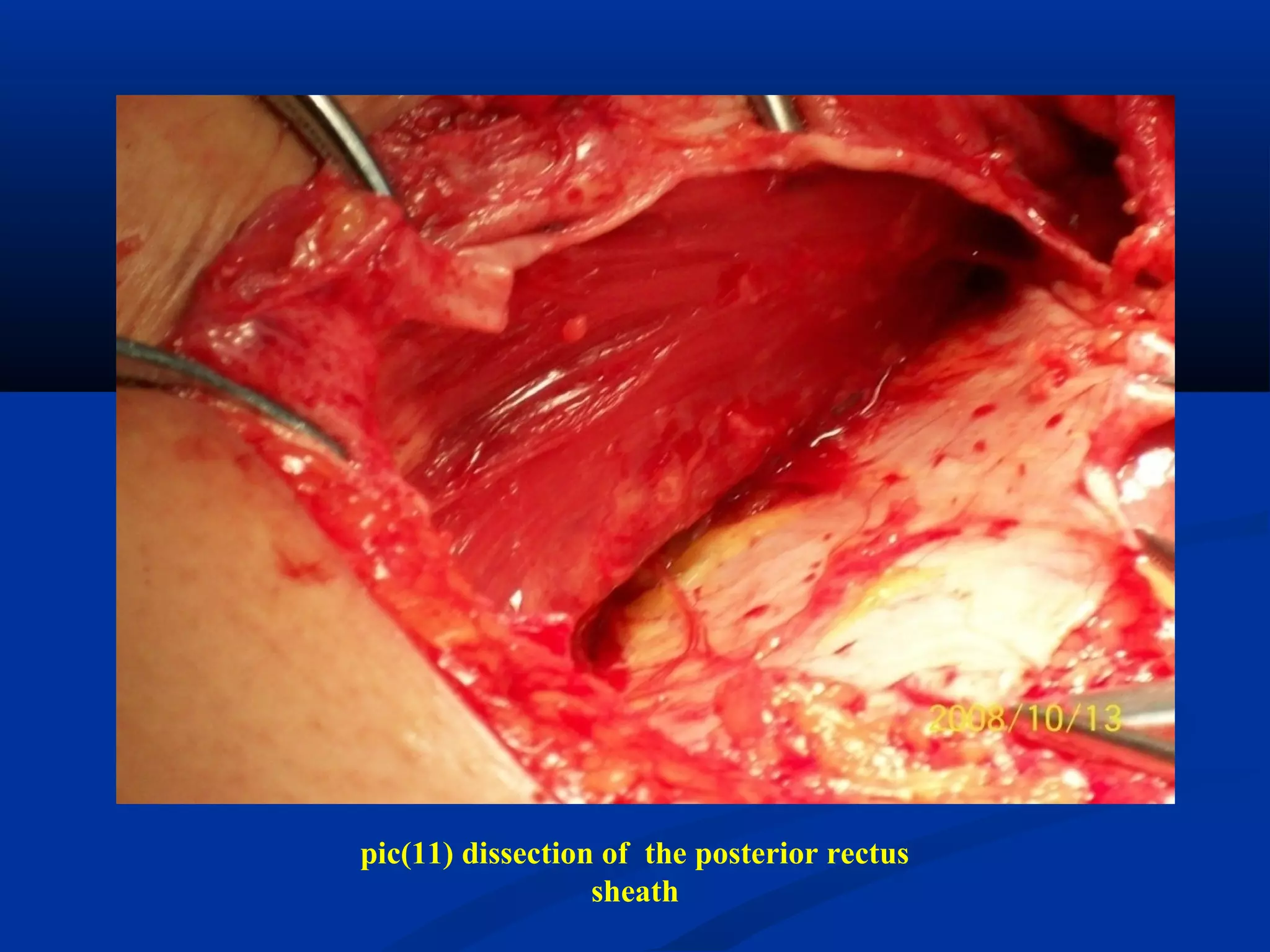
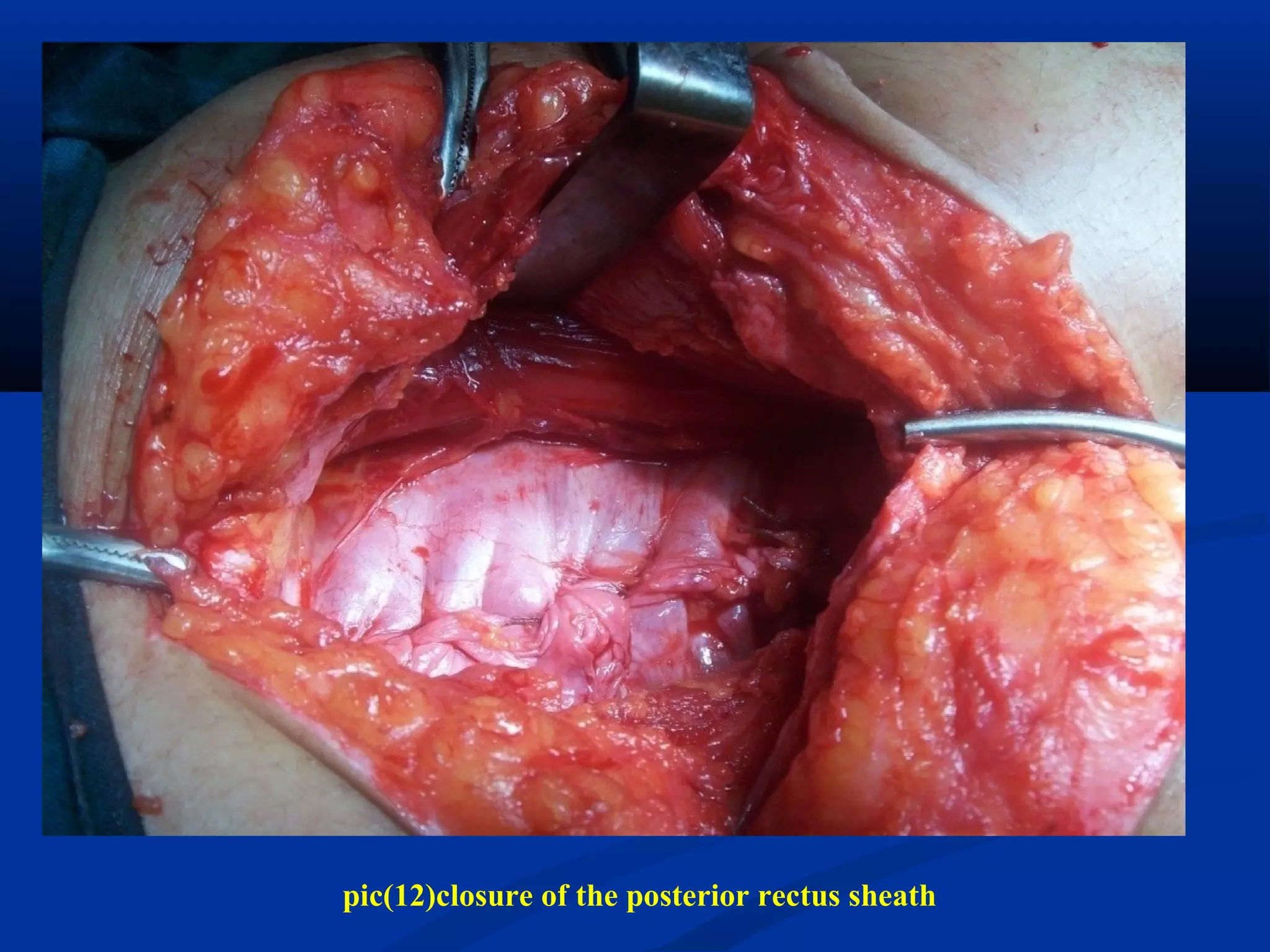
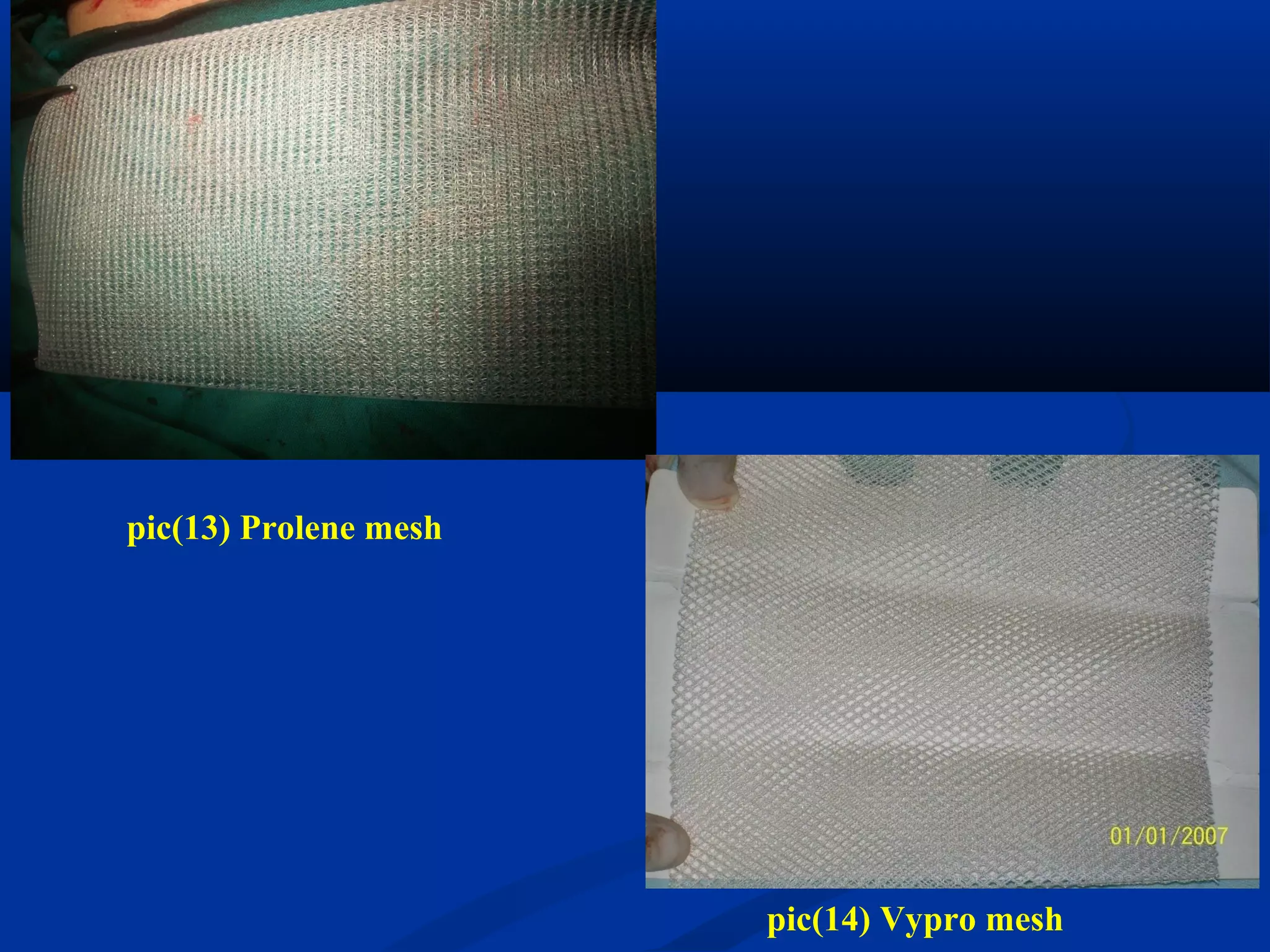
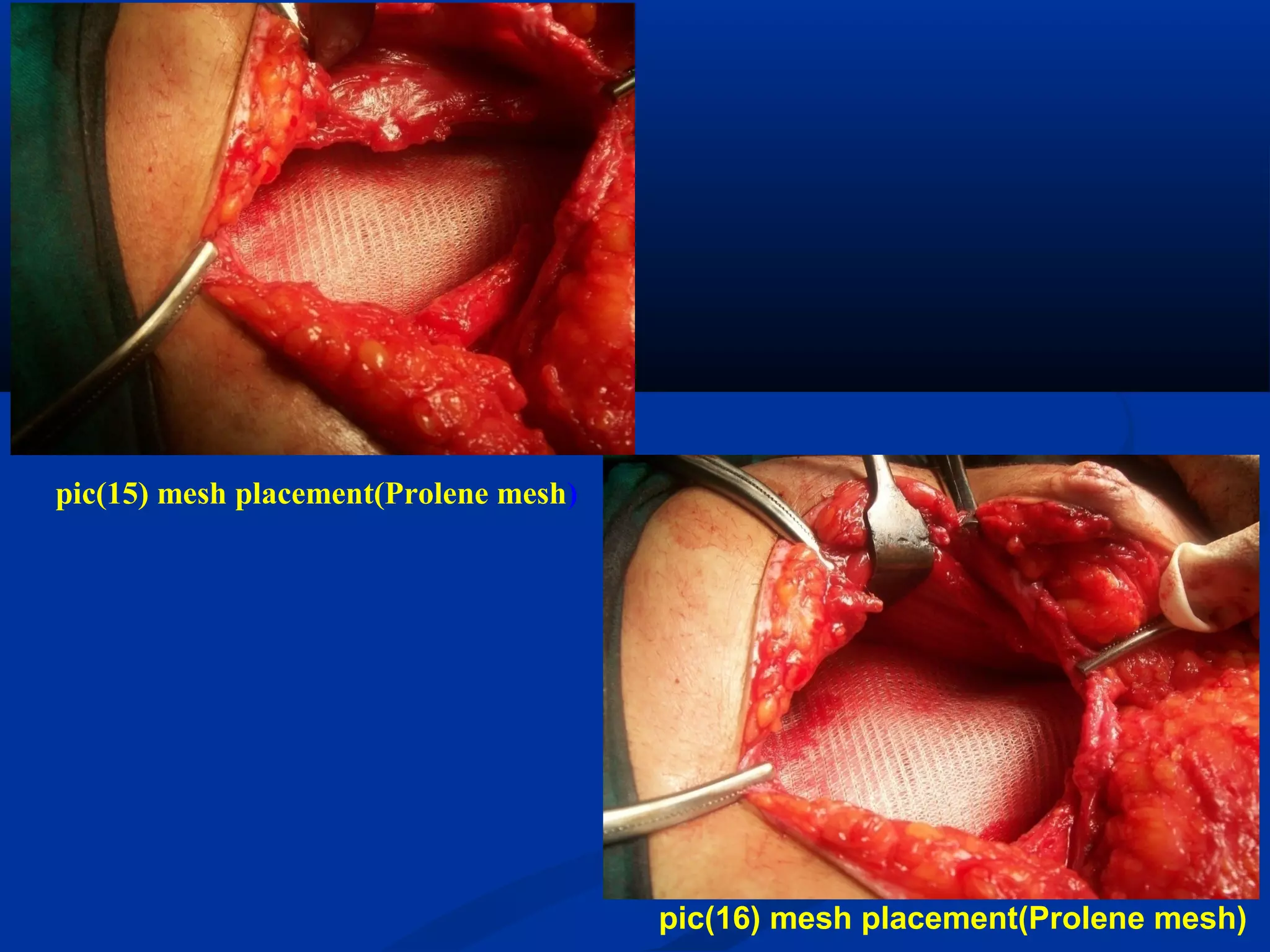
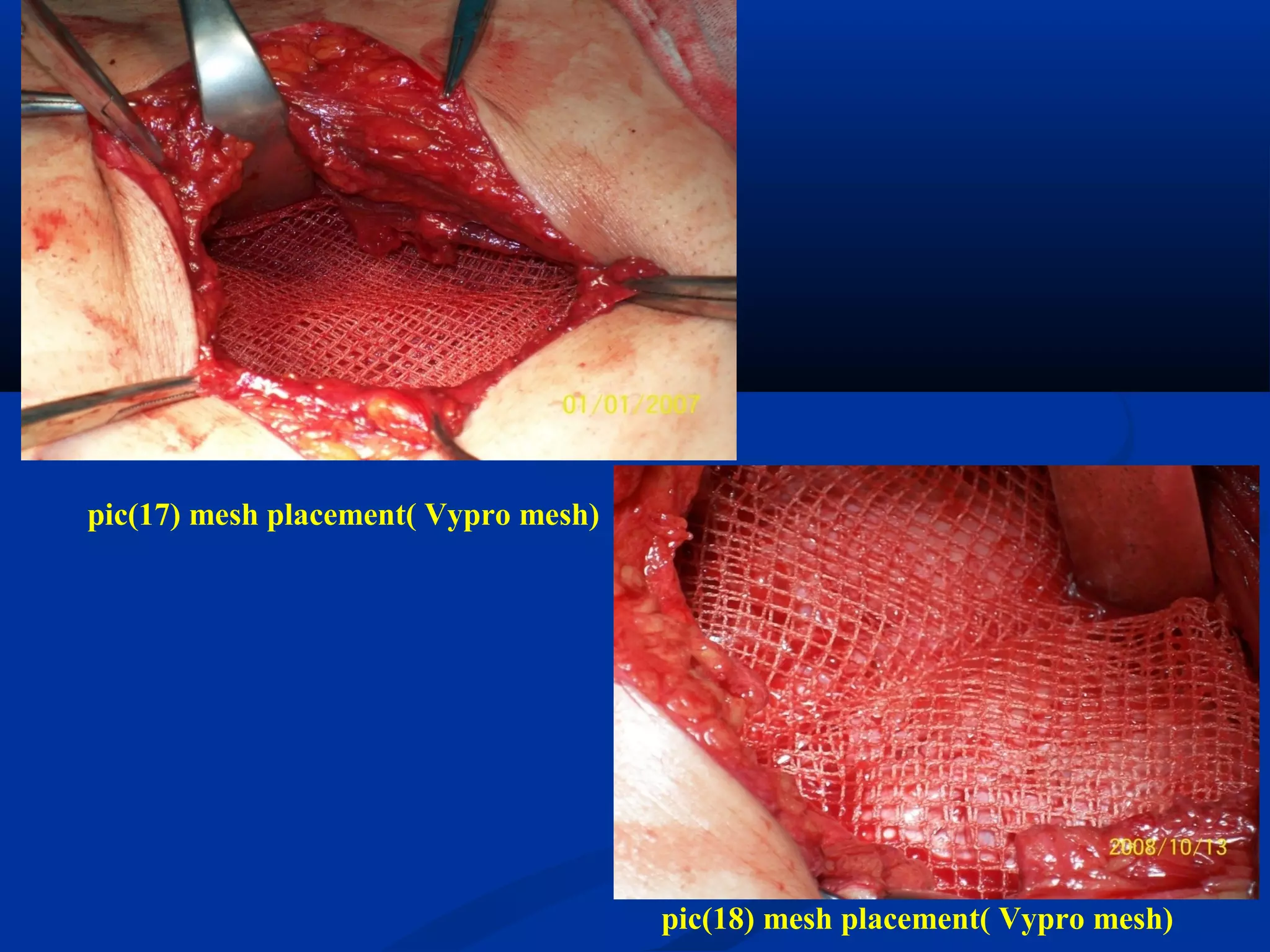
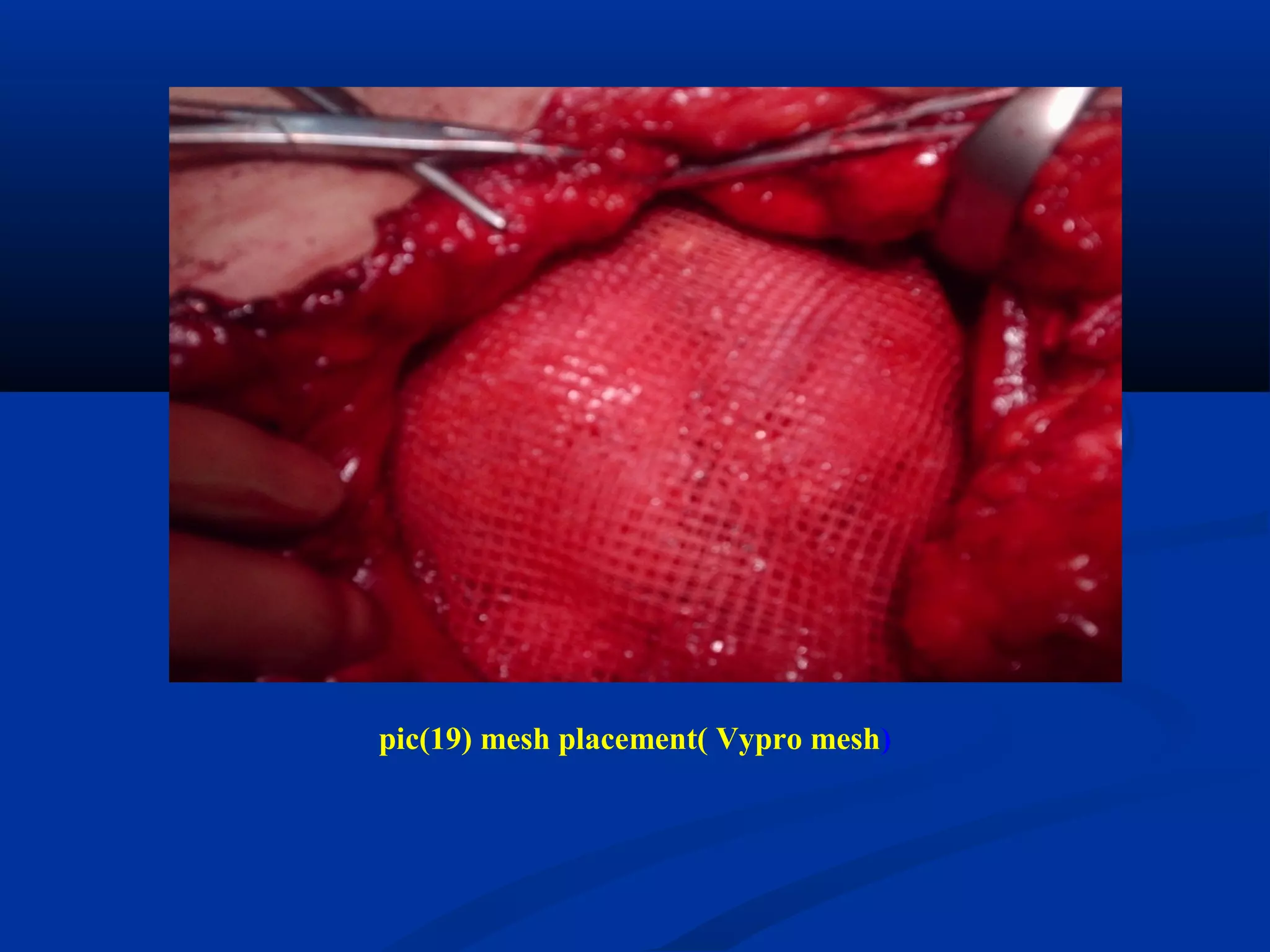
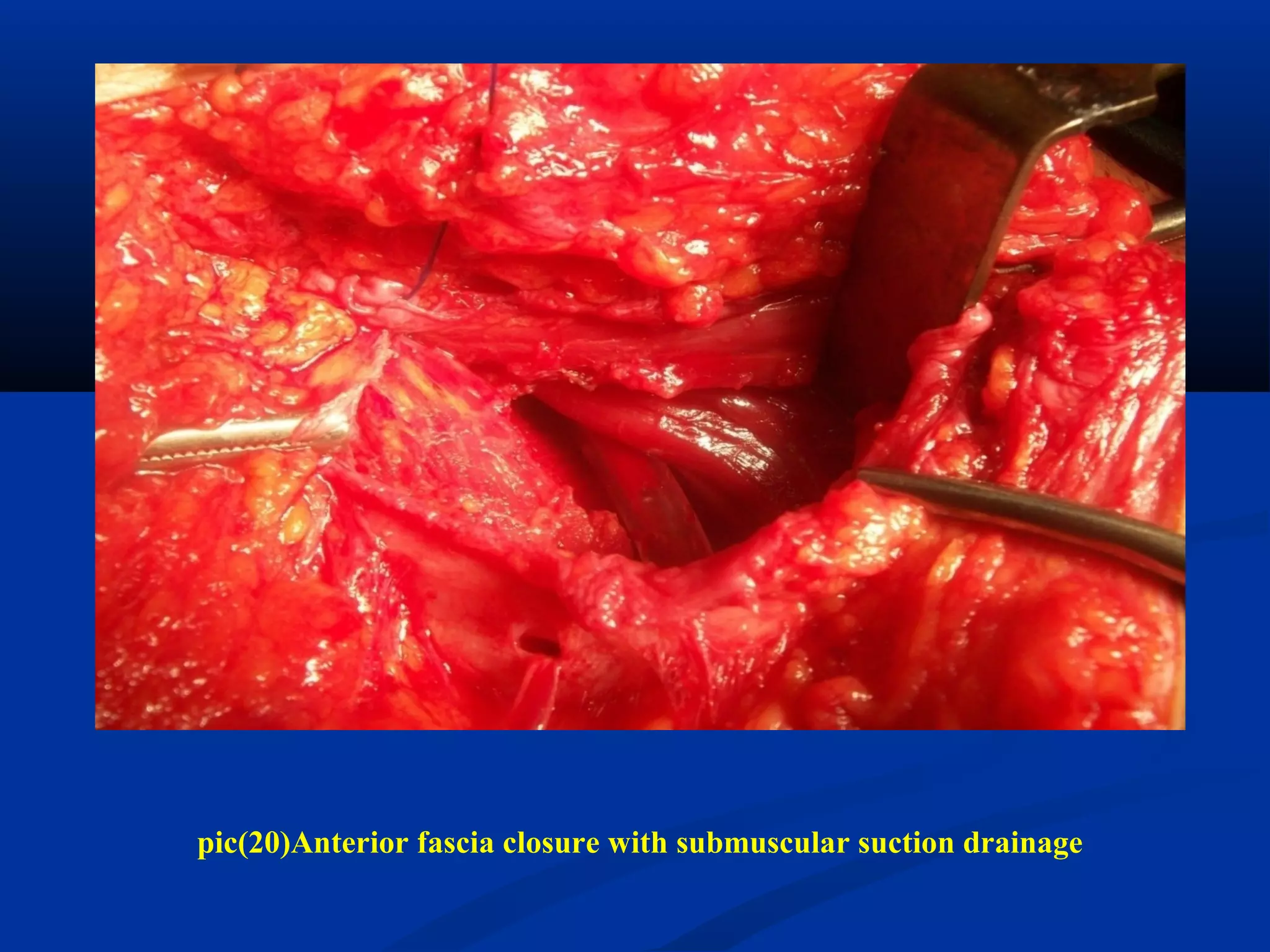
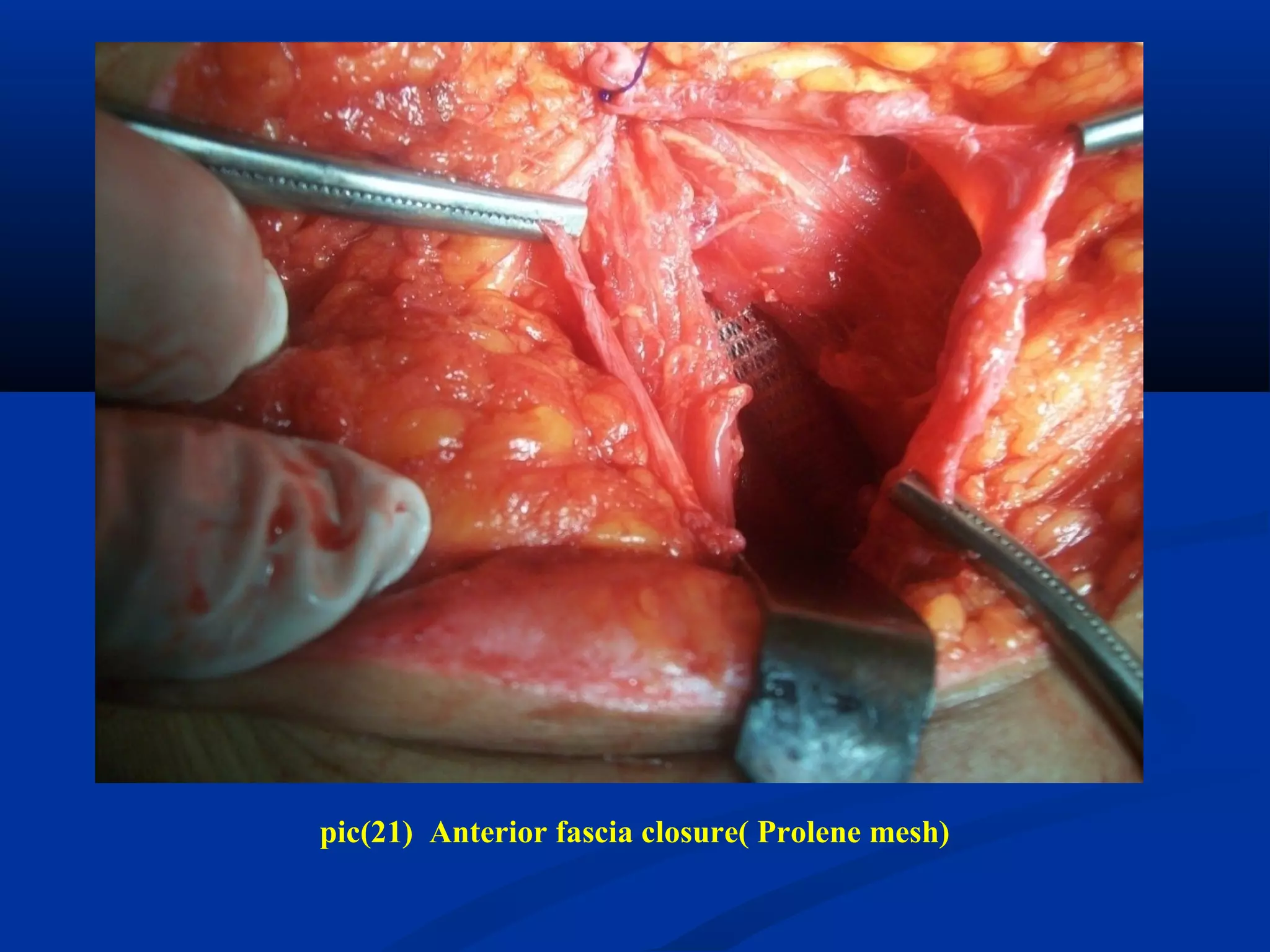
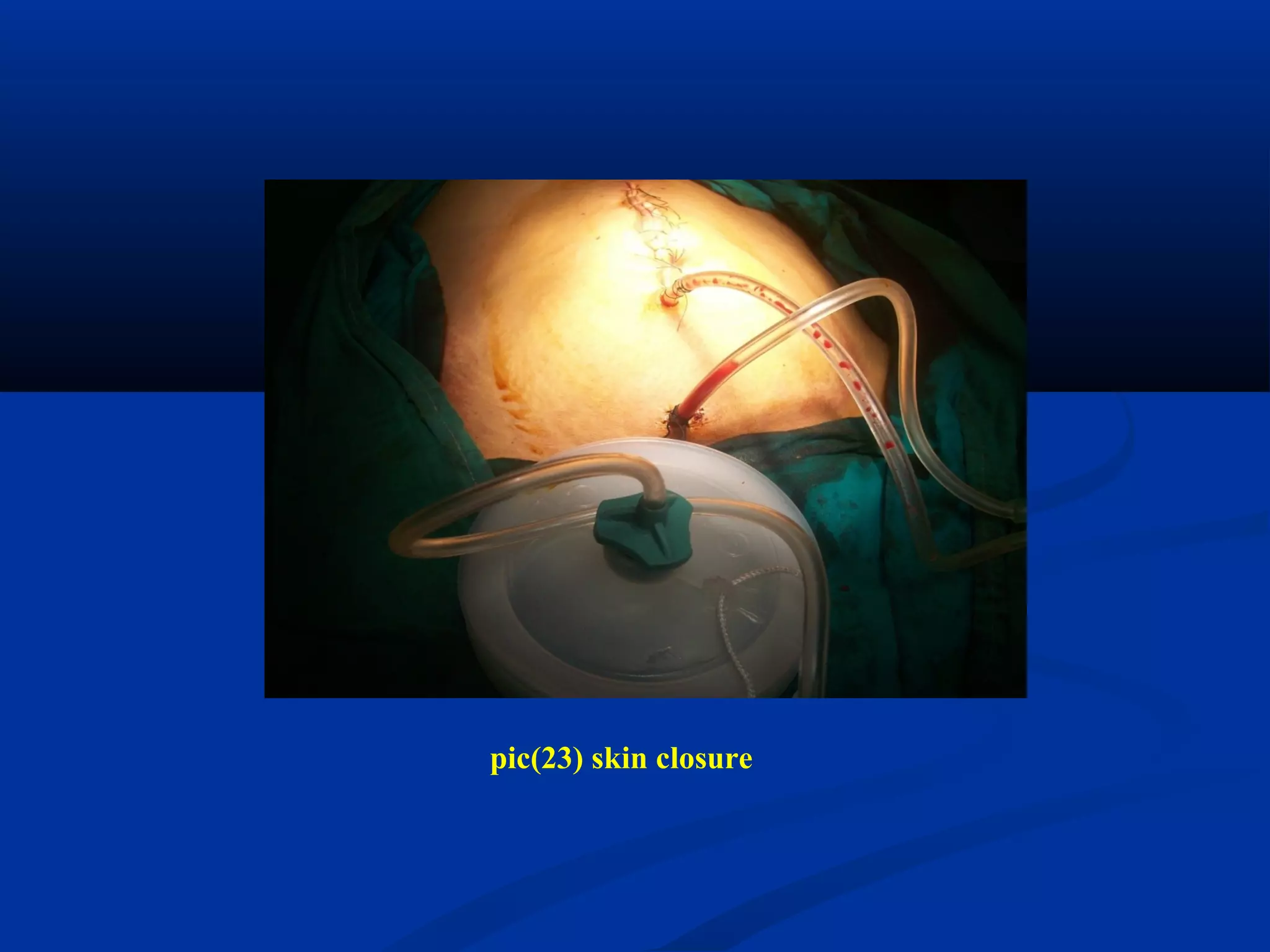
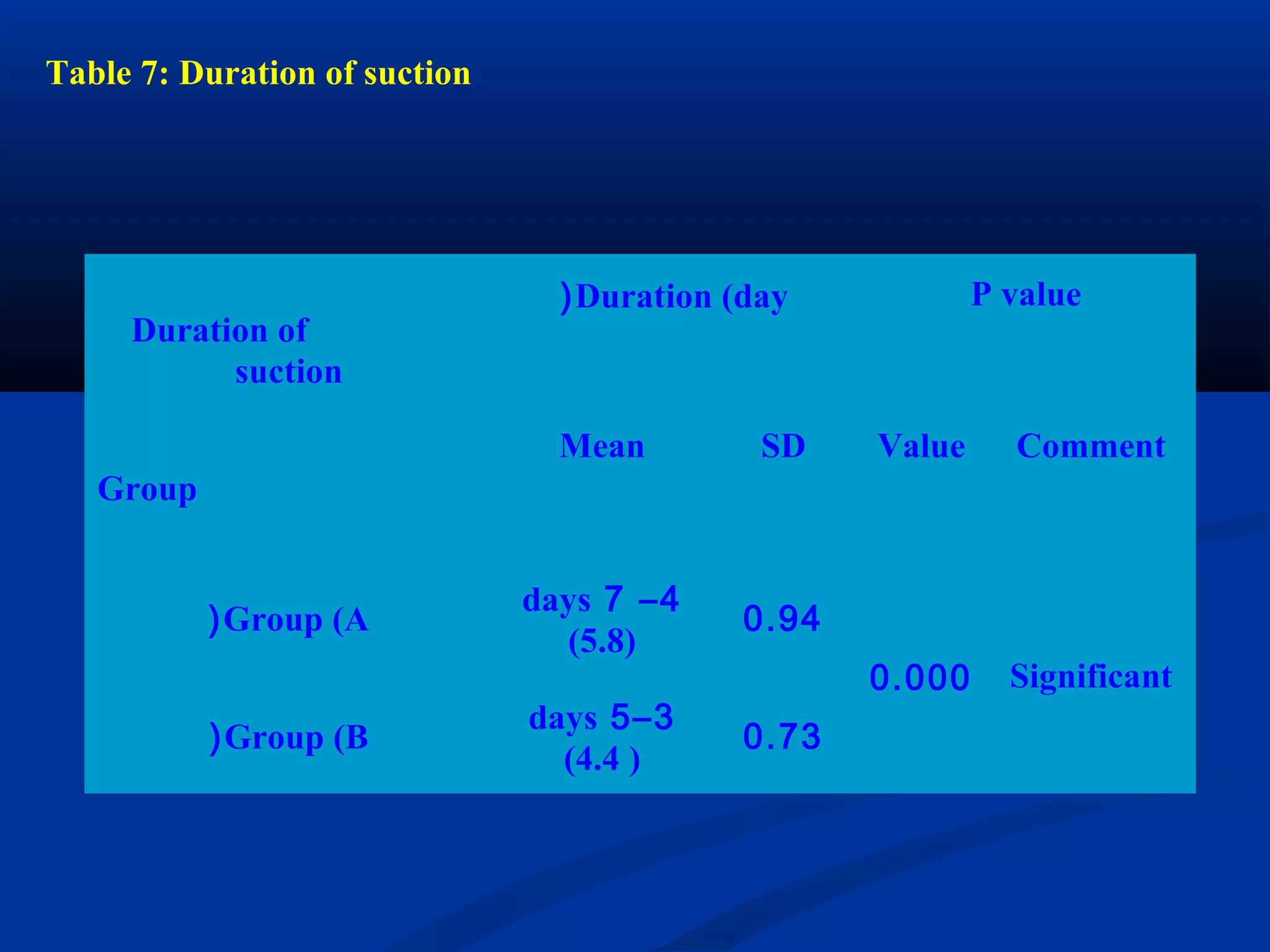
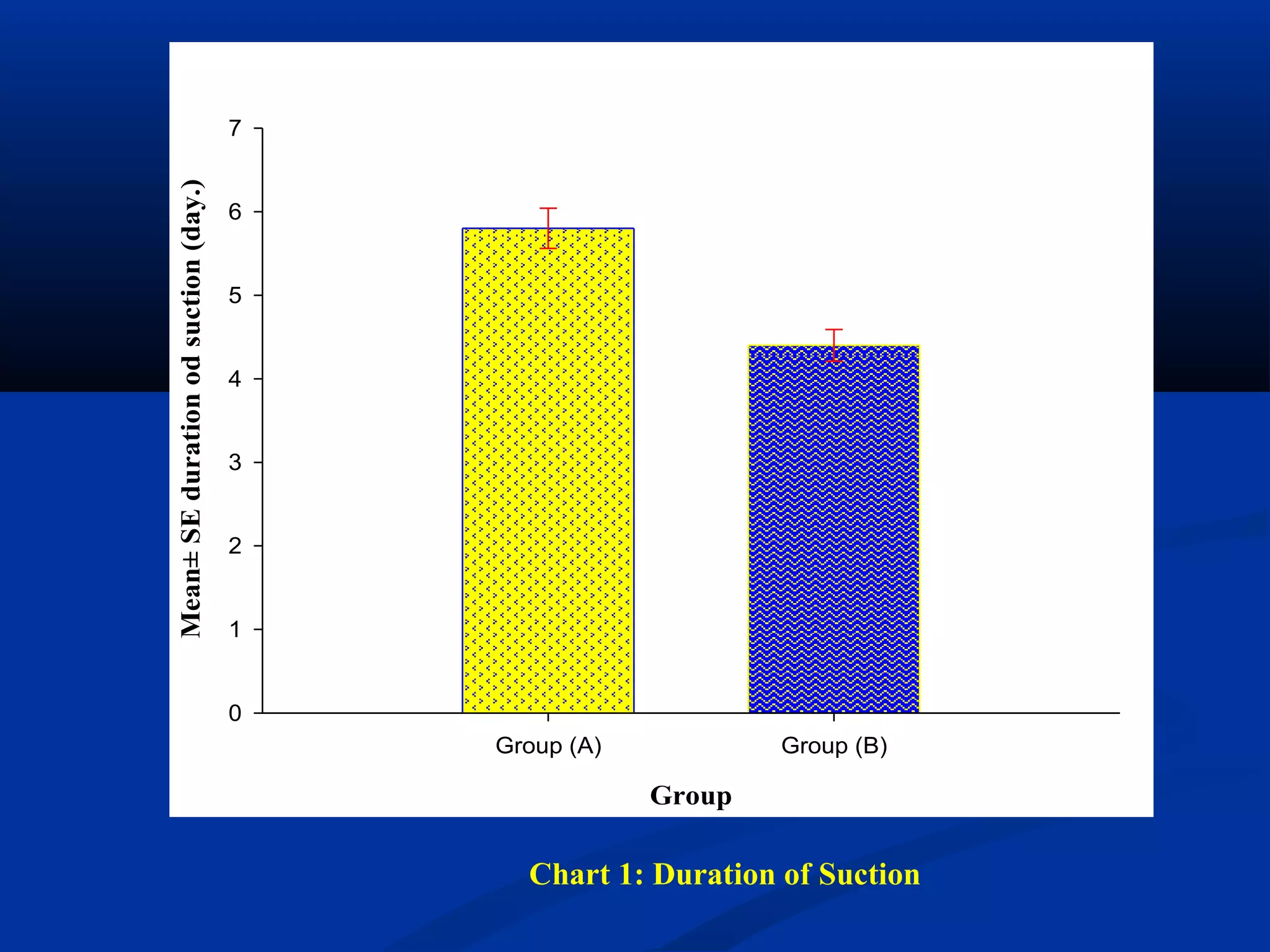
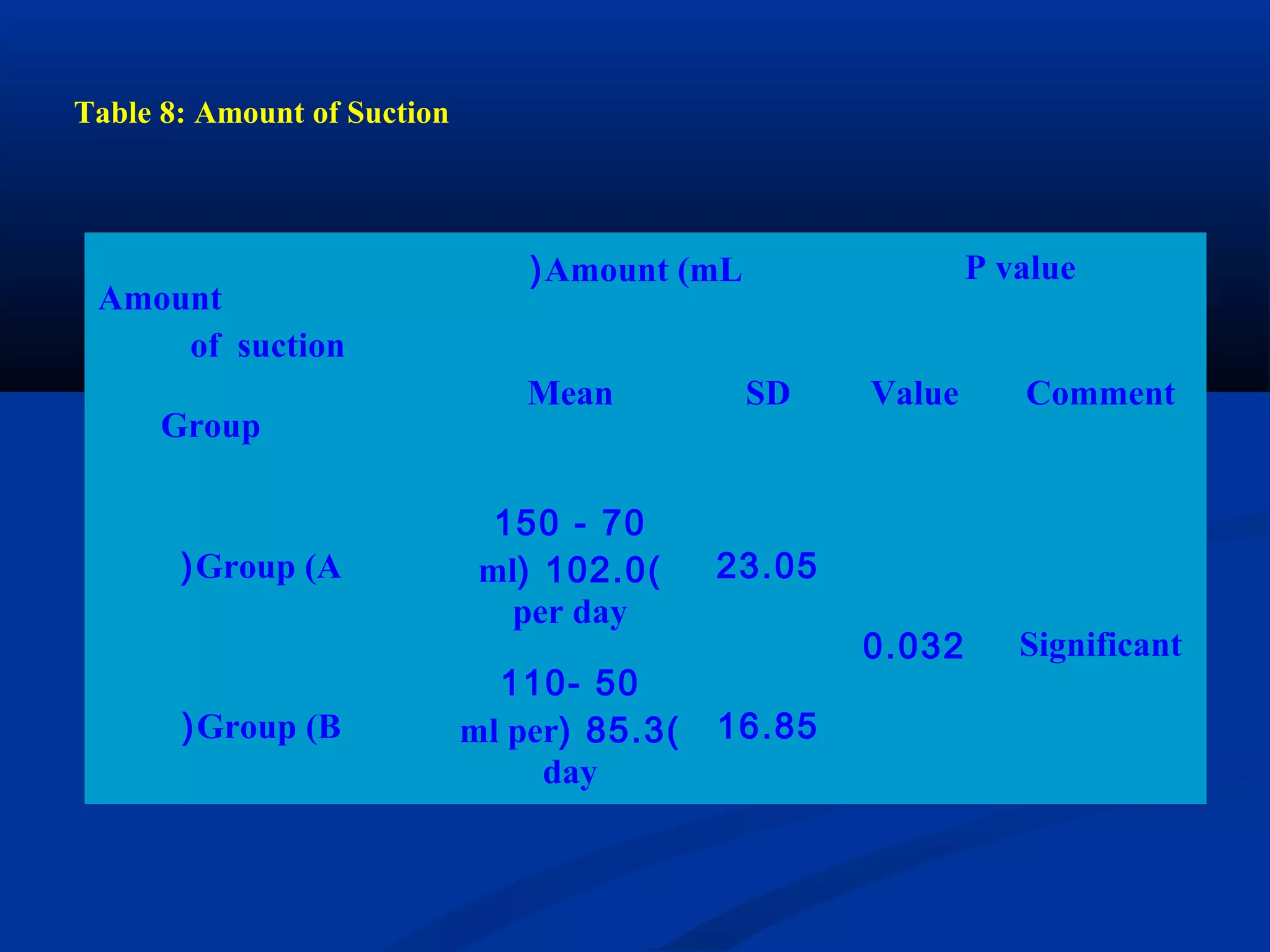
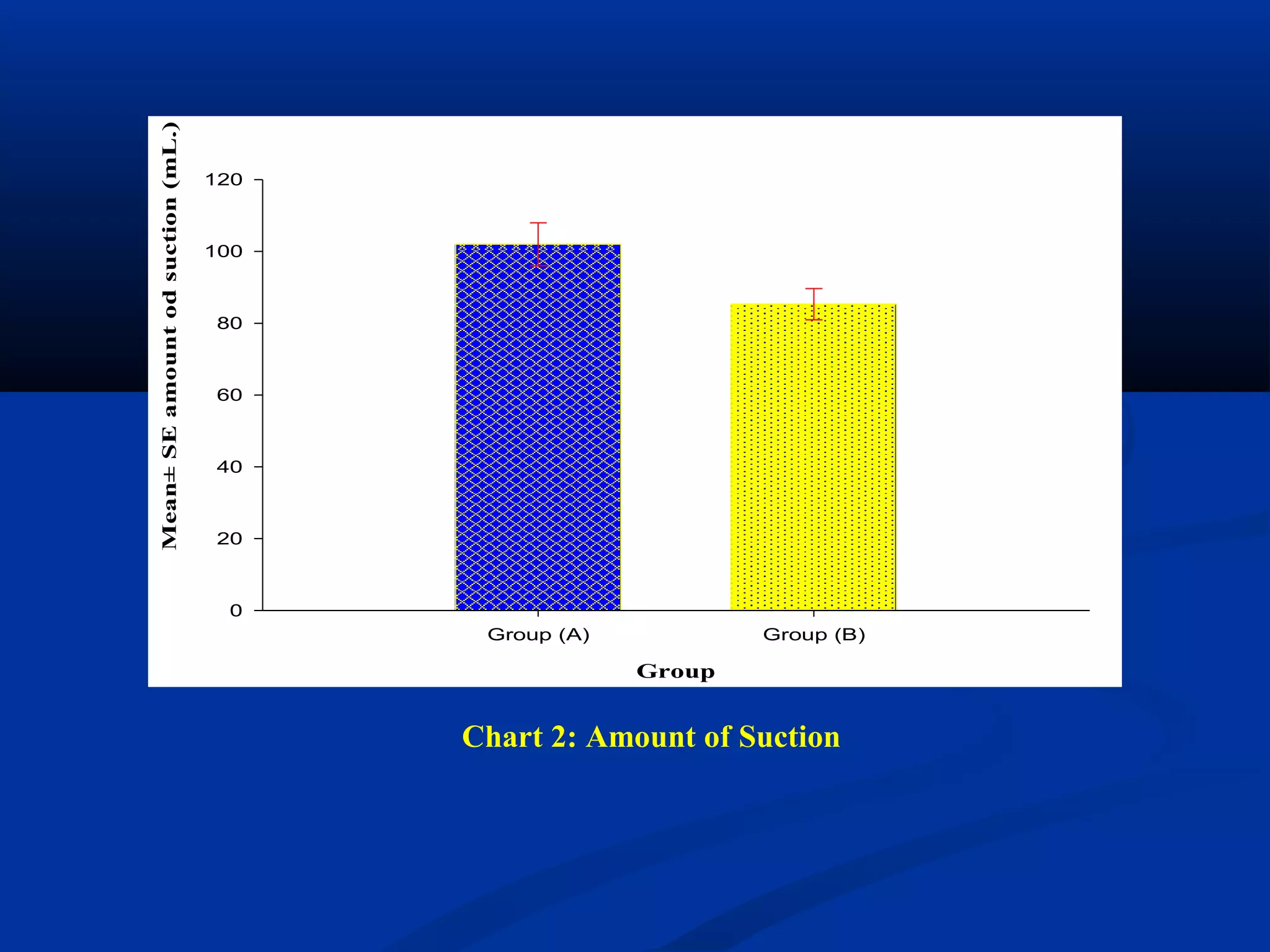
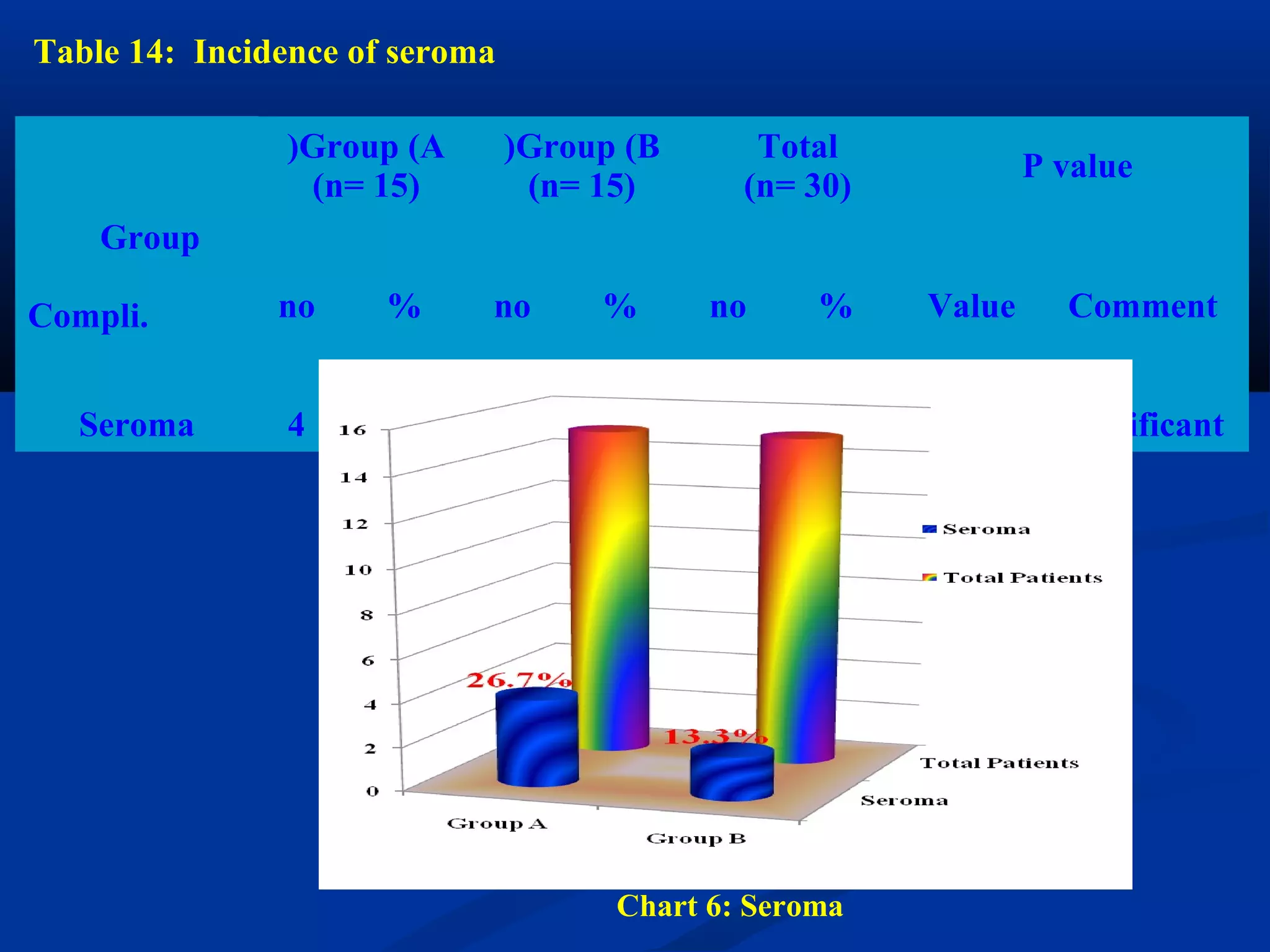
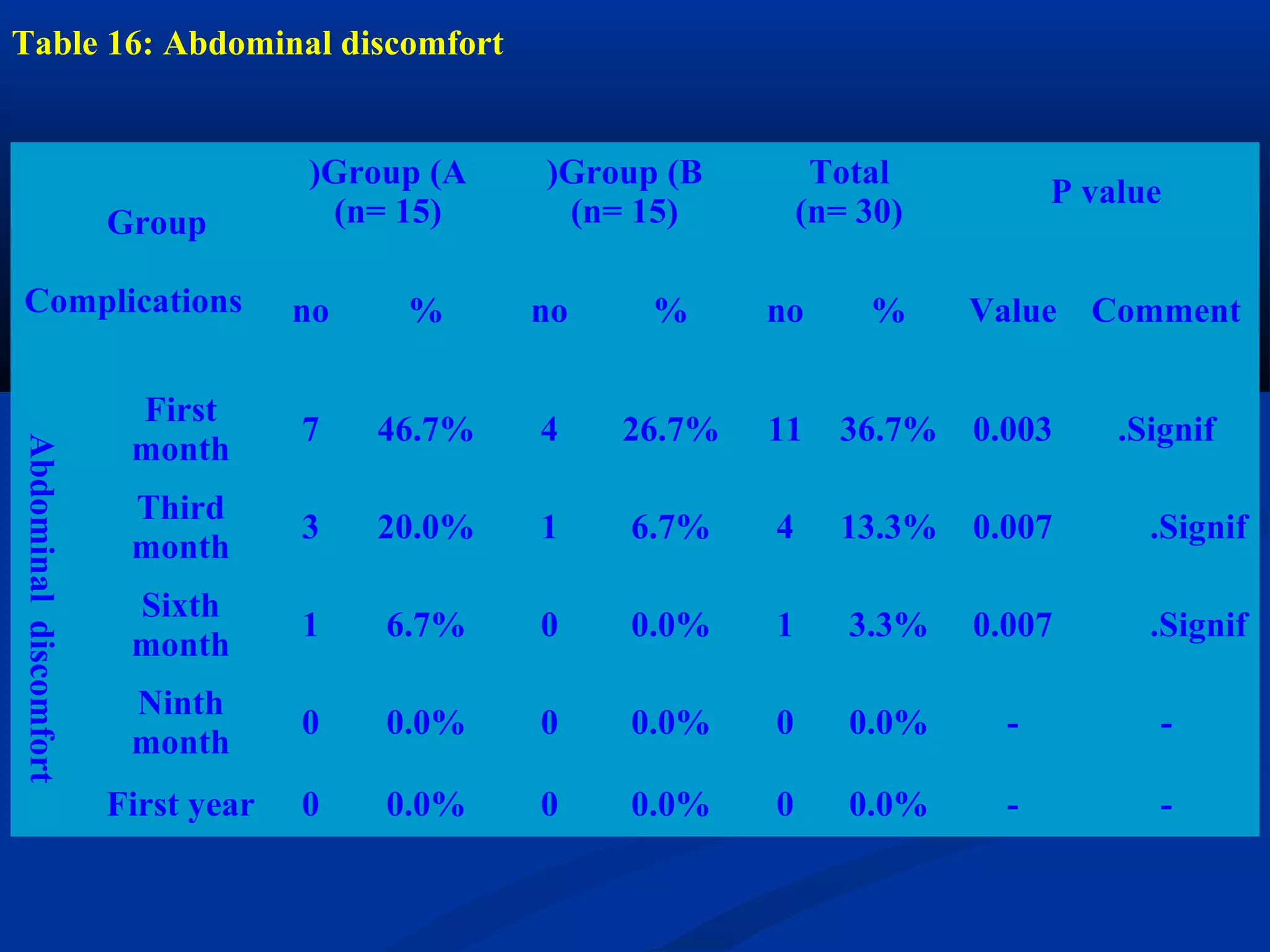
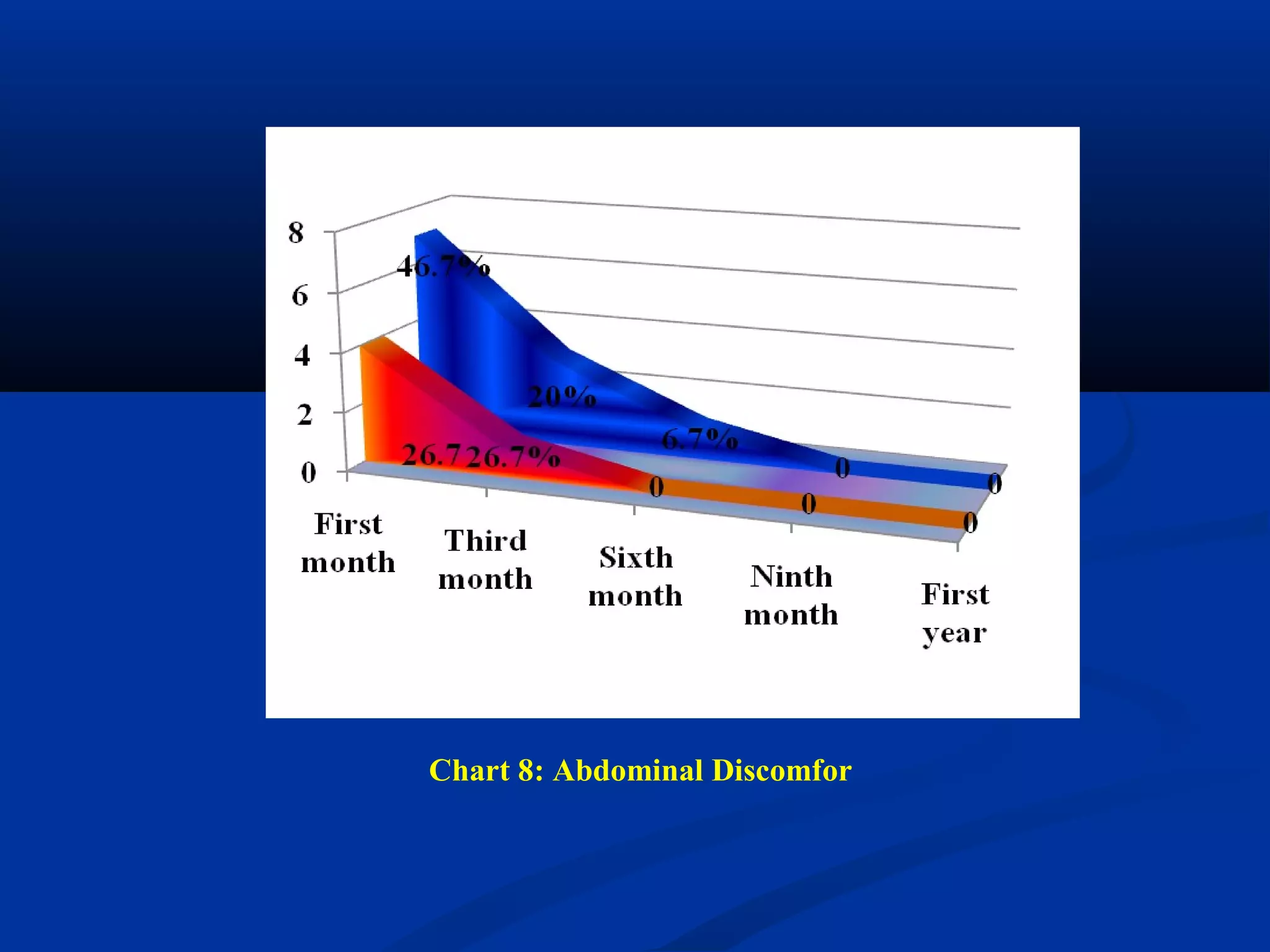
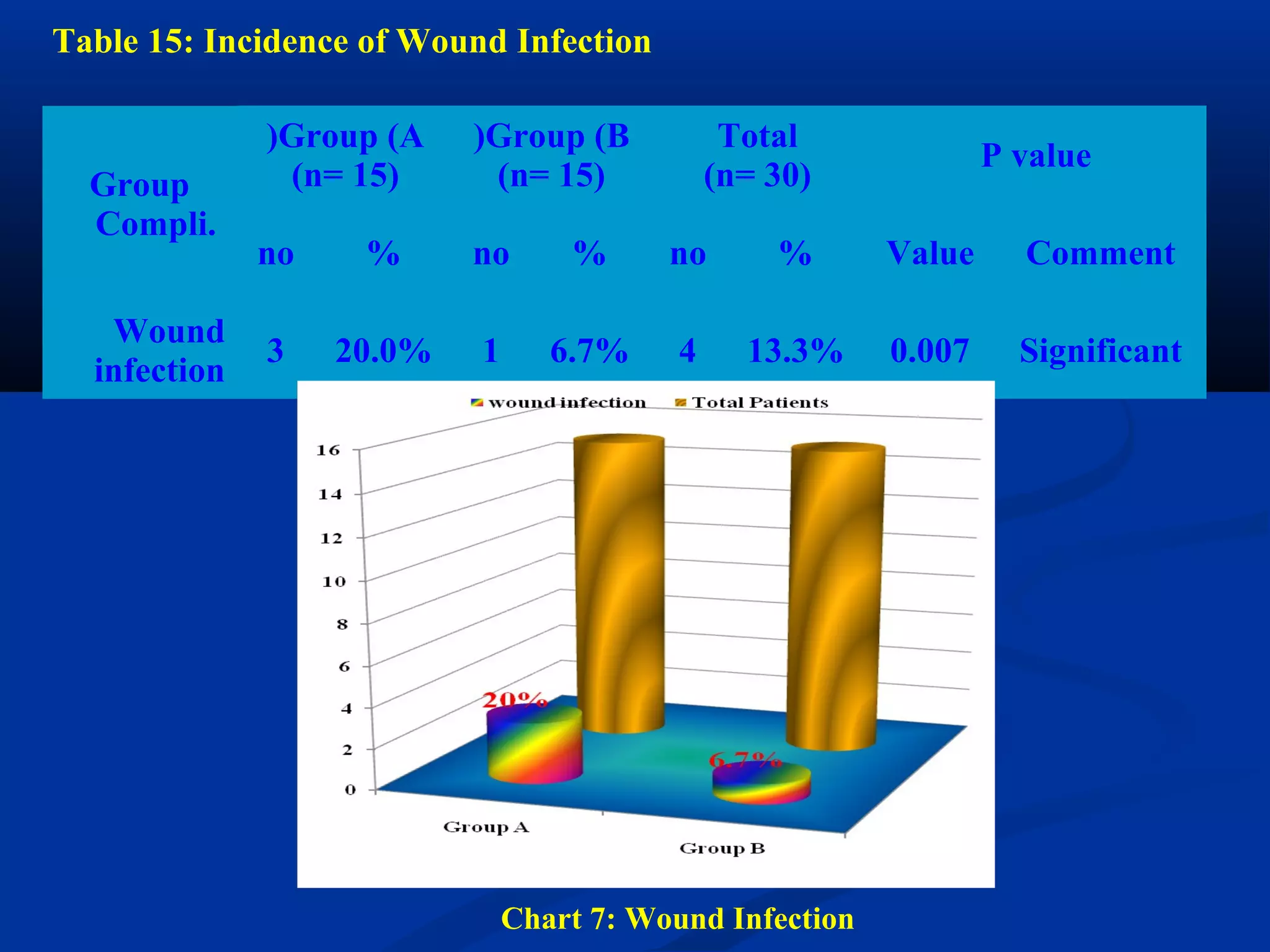
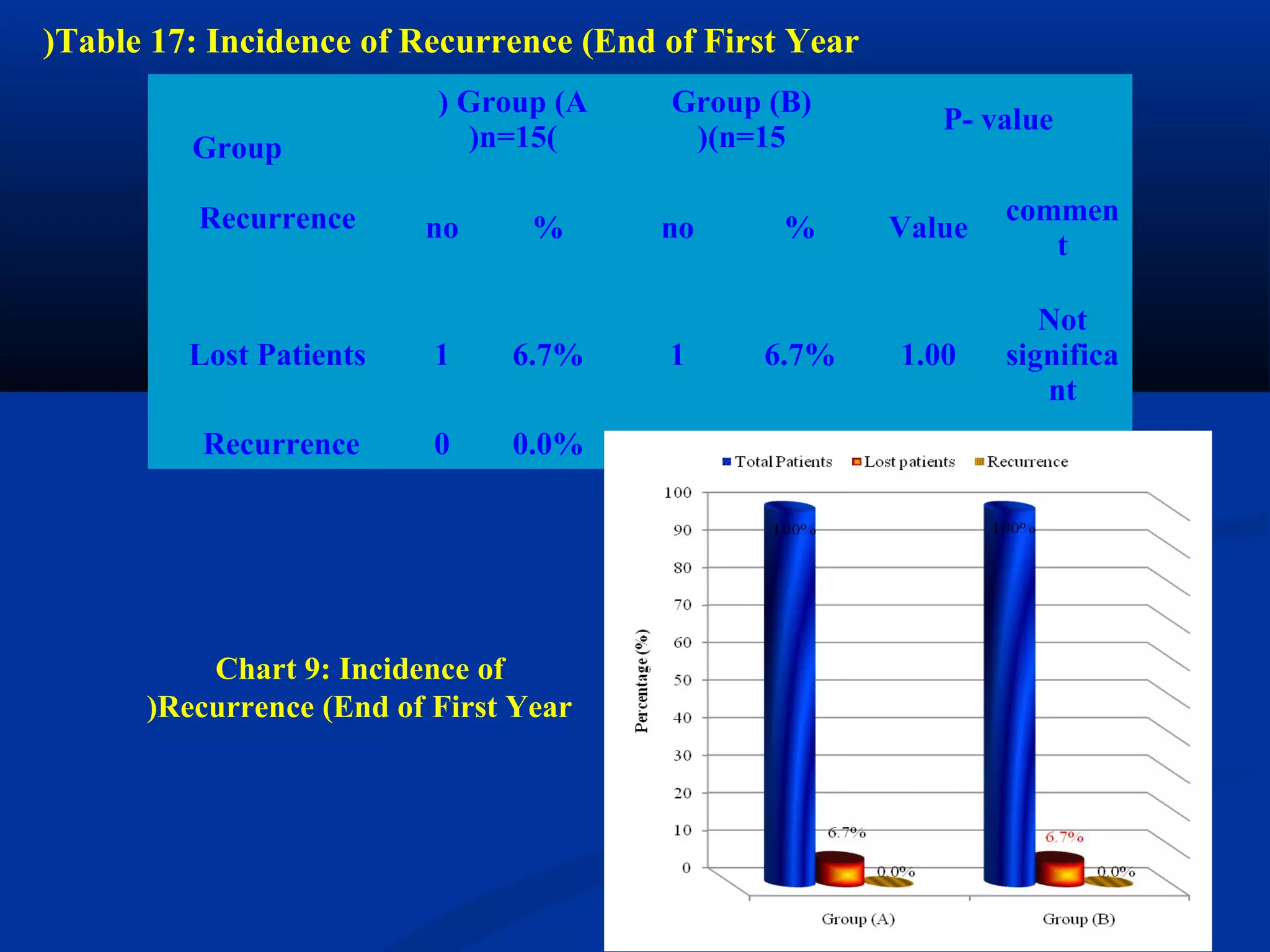
This document discusses a study that evaluated the sublay retromuscular technique for ventral incisional hernia repair using lightweight Vypro mesh versus standard heavyweight Prolene mesh. 30 patients with moderate sized hernias were divided into two groups, with one group receiving Vypro mesh and the other receiving Prolene mesh via the sublay retromuscular technique. The study aims to compare postoperative complications, chronic pain, and recurrence rates between the two mesh types.