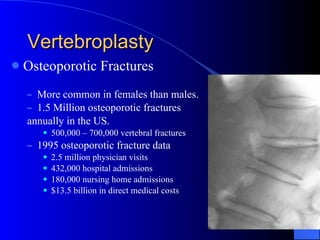
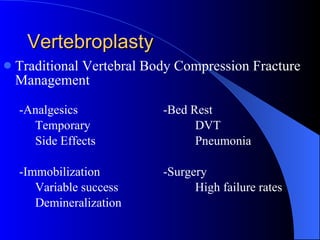
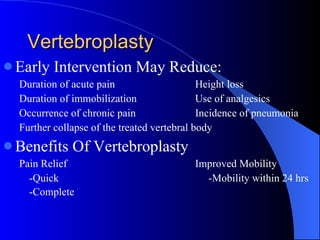
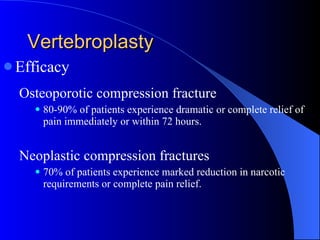
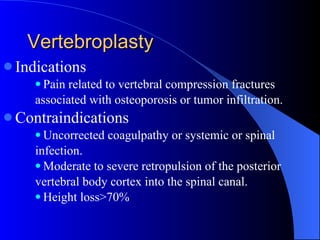
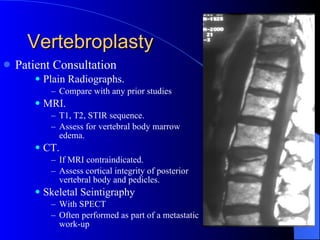
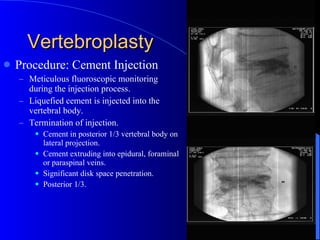
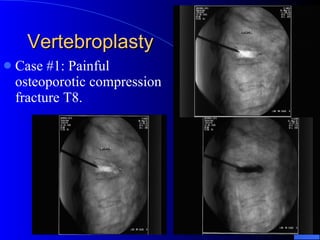
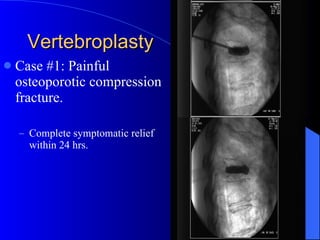
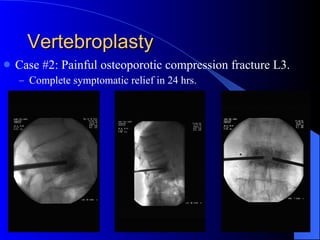
Vertebroplasty is a minimally invasive procedure for treating painful vertebral compression fractures, providing immediate pain relief and preventing further vertebral collapse. Historically, it utilizes acrylic bone cement and has efficacy rates of 80-90% for osteoporotic fractures and 70% for neoplastic fractures, with low complication rates. Patient selection is crucial, focusing on recent fractures and excluding those with contraindications such as uncorrected coagulopathy or severe spinal canal encroachment.