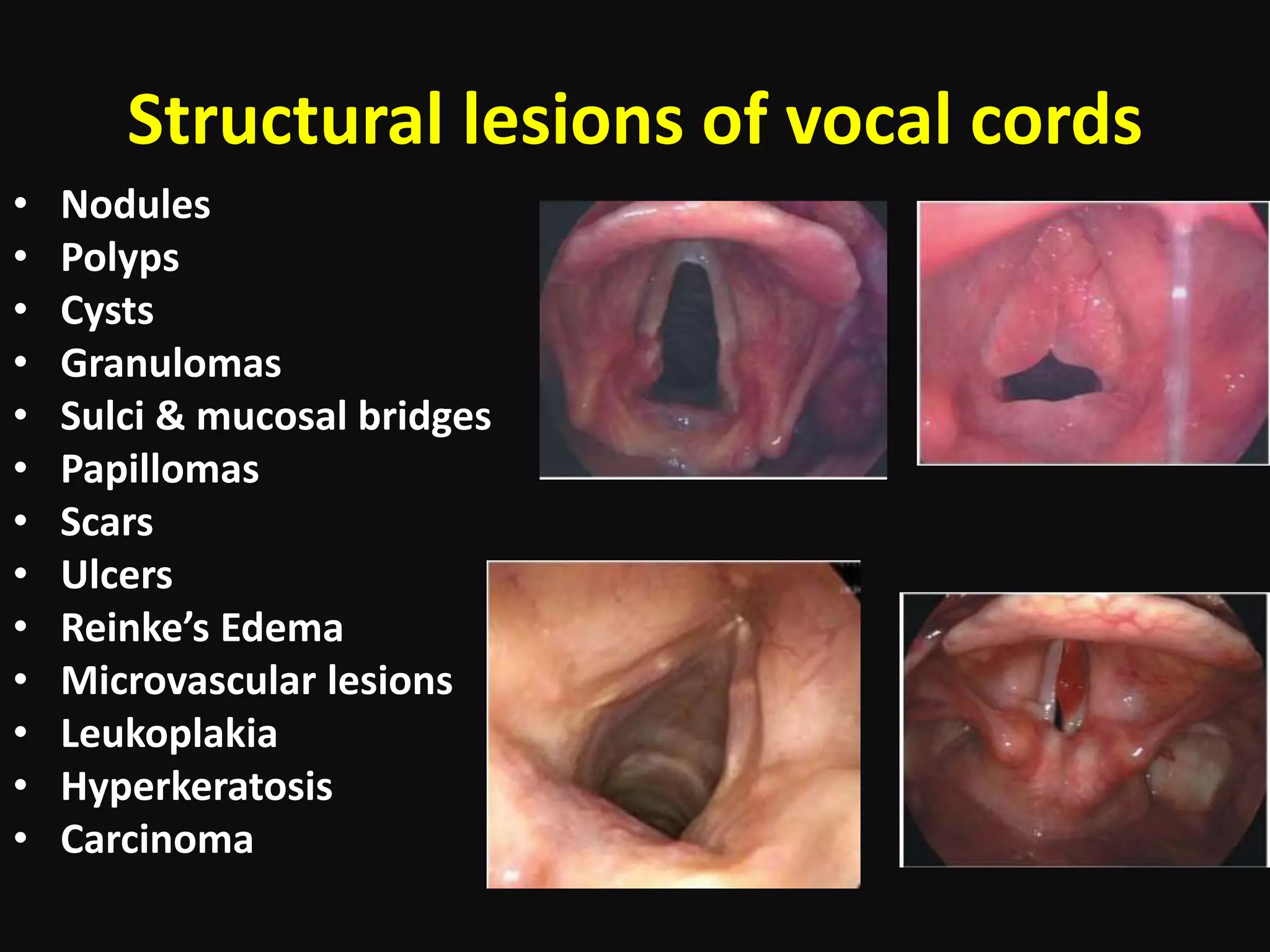
The document outlines the anatomy, causes, and treatment of pre-malignant lesions of the vocal cords, emphasizing the importance of early diagnosis and management to prevent progression to laryngeal cancer. Key concepts include various structural lesions, their clinical presentation, and the principles of phonomicrosurgery aimed at preserving vocal quality. Treatment options range from vocal hygiene and therapy to surgical interventions, with a focus on careful surgical techniques to mitigate complications.