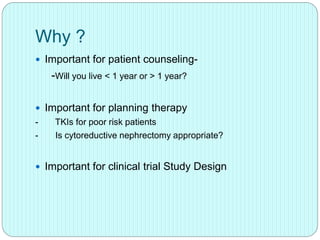
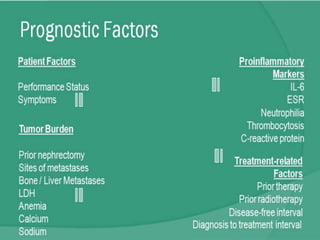
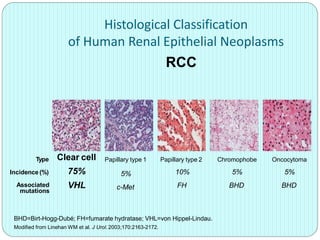
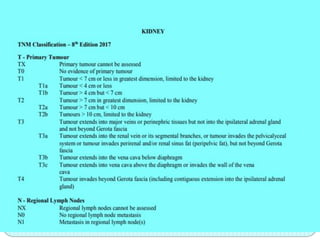
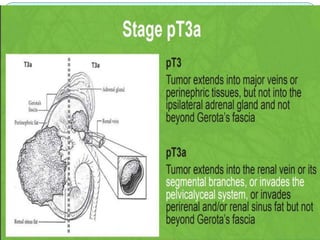
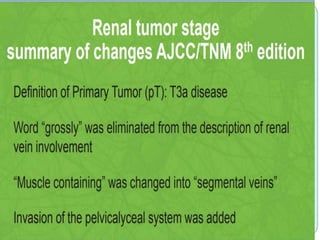
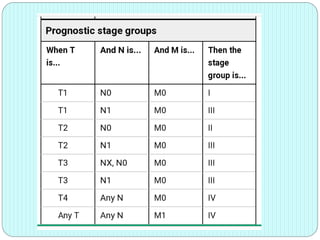
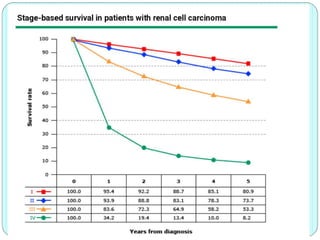
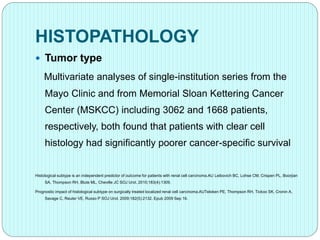
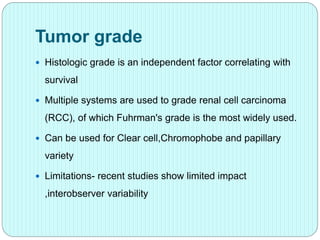
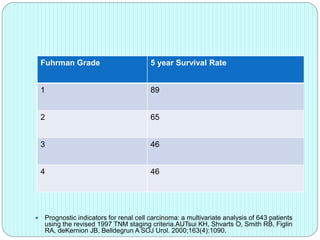
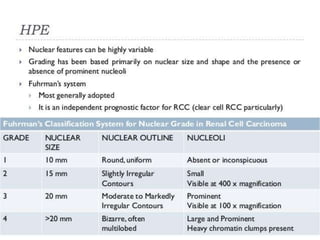
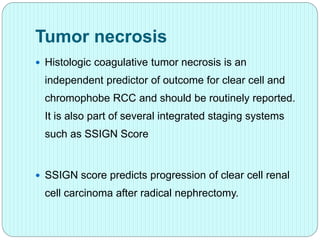
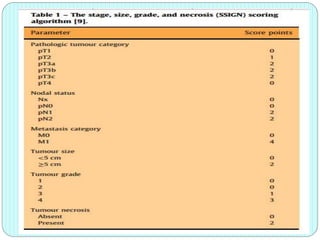
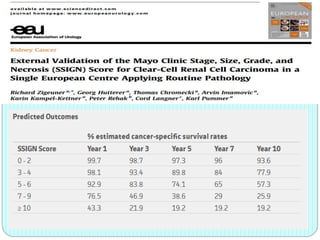
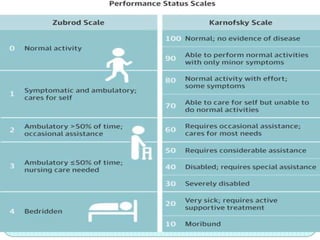
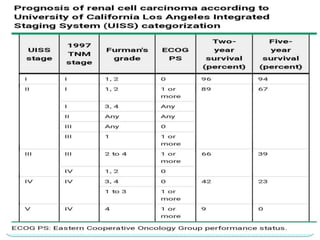
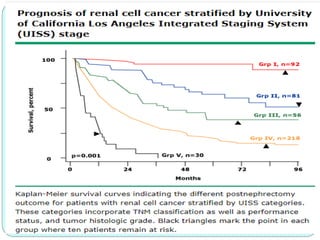
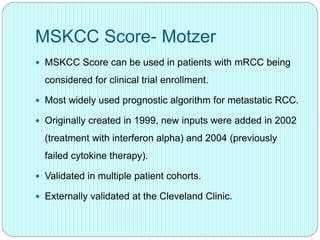
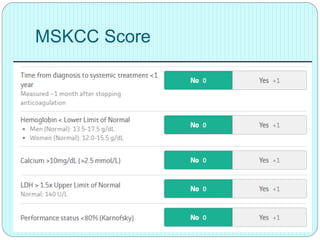
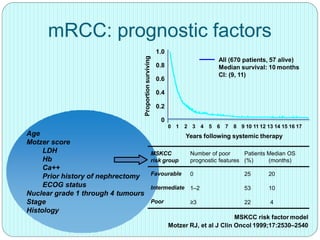
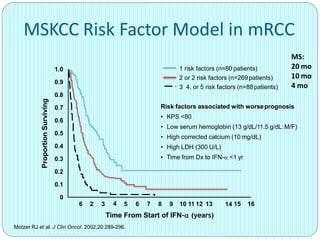
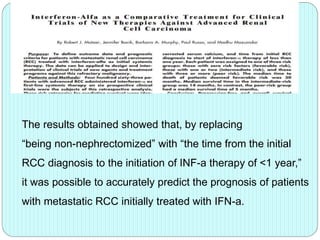
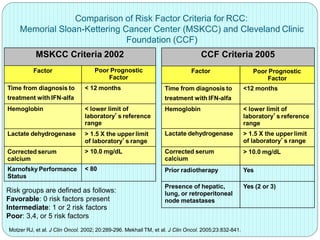
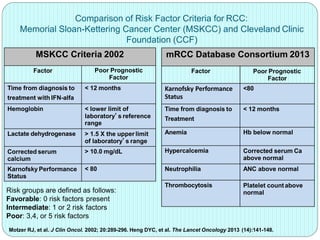
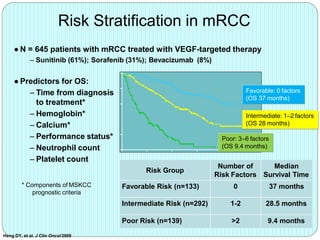
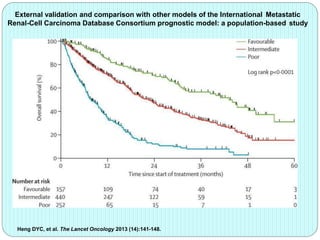
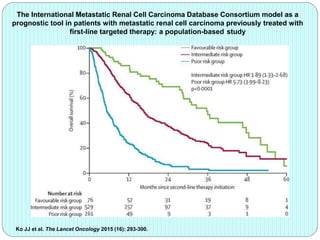
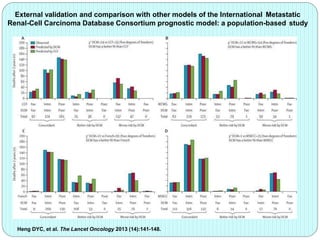
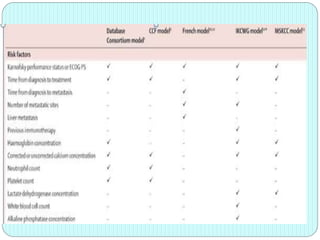
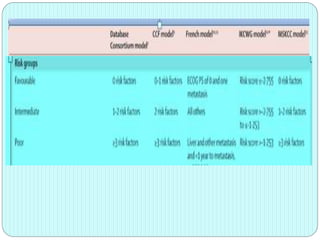
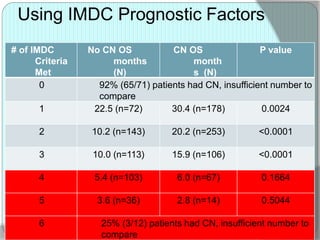
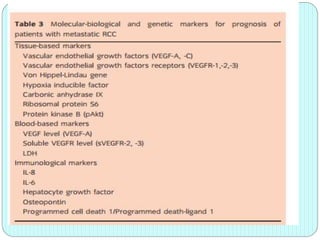
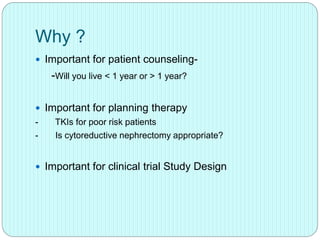
The document outlines risk stratification in renal cell carcinoma, discussing important prognostic factors, histopathological classifications, and established criteria such as the MSKCC and Heng models. It emphasizes the significance of accurate risk assessment for patient counseling, therapy planning, and clinical trial design. While current models have limitations and clinical applications are insufficient, advancements in molecular-targeted therapies show promise in improving patient outcomes.