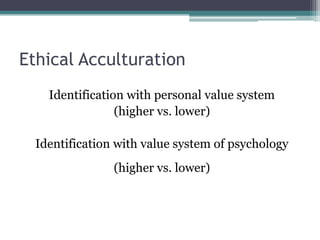
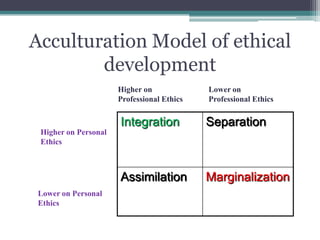
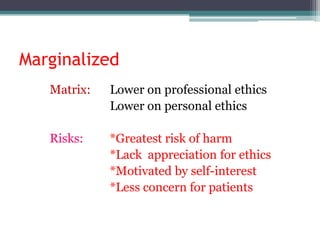
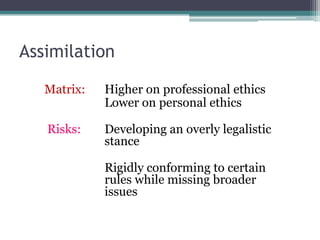
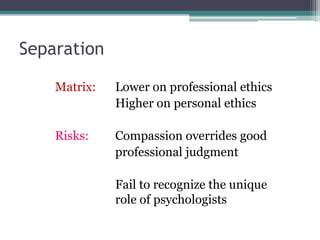
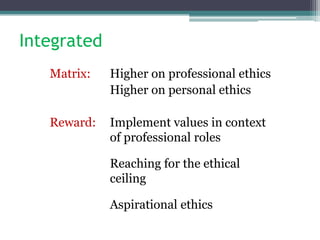
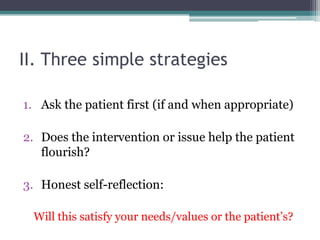
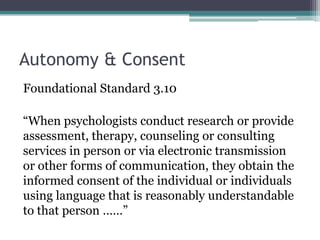
This document outlines a presentation on unlearning received wisdom in ethics. It discusses using an acculturation model to integrate personal and professional ethics through higher identification with both. Three strategies are presented: asking patients, focusing on patient flourishing, and honest self-reflection. Five ethical principles - autonomy, beneficence, nonmaleficence, fidelity, and justice - provide a framework. Unhealthy strategies like overemphasizing rules without principles are discussed. The presentation involves examining examples of received wisdom that may not be helpful, like assumptions about informed consent, self-disclosure, and referral practices. It aims to have participants thoughtfully evaluate common beliefs through discussion.