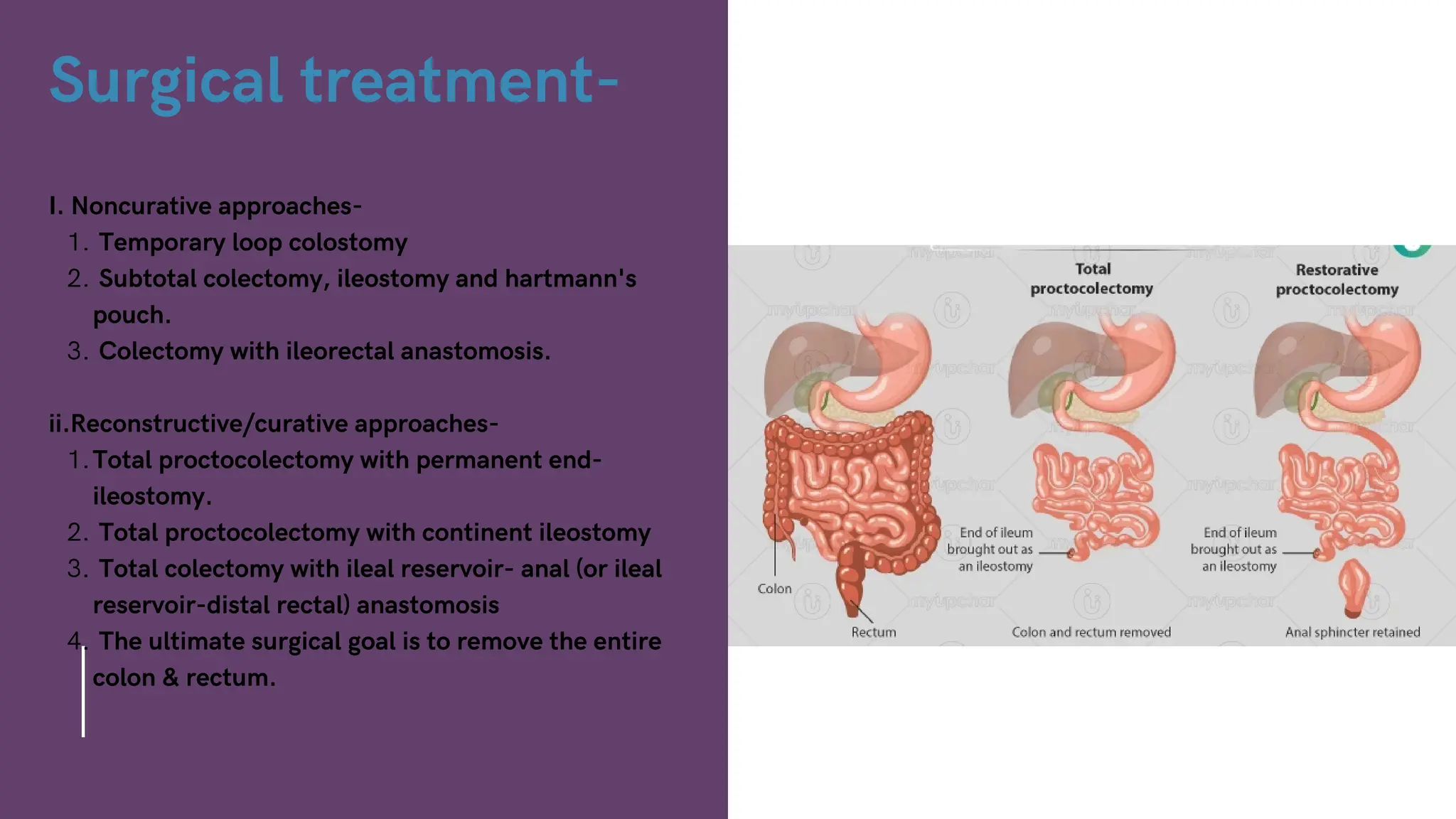
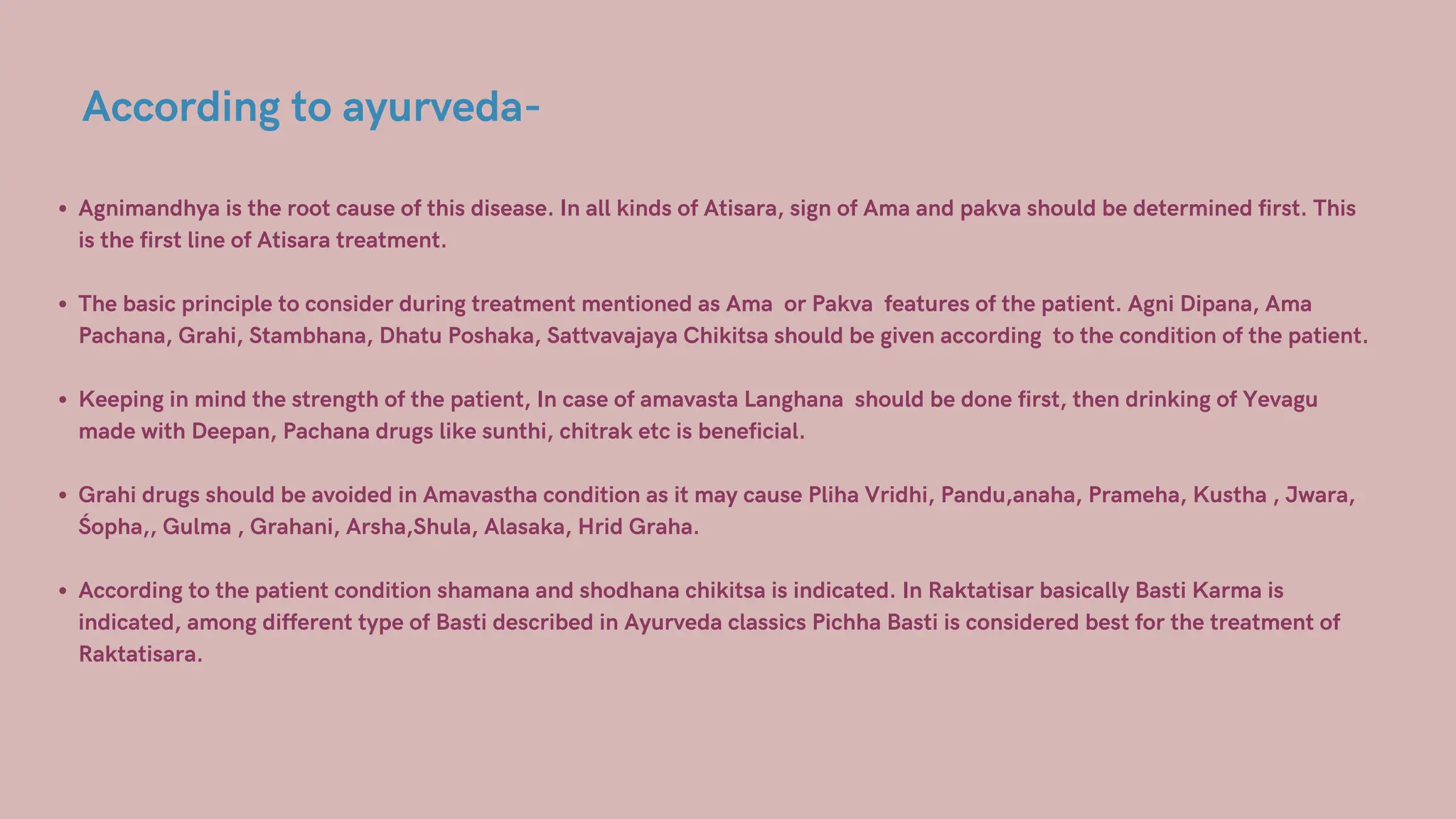
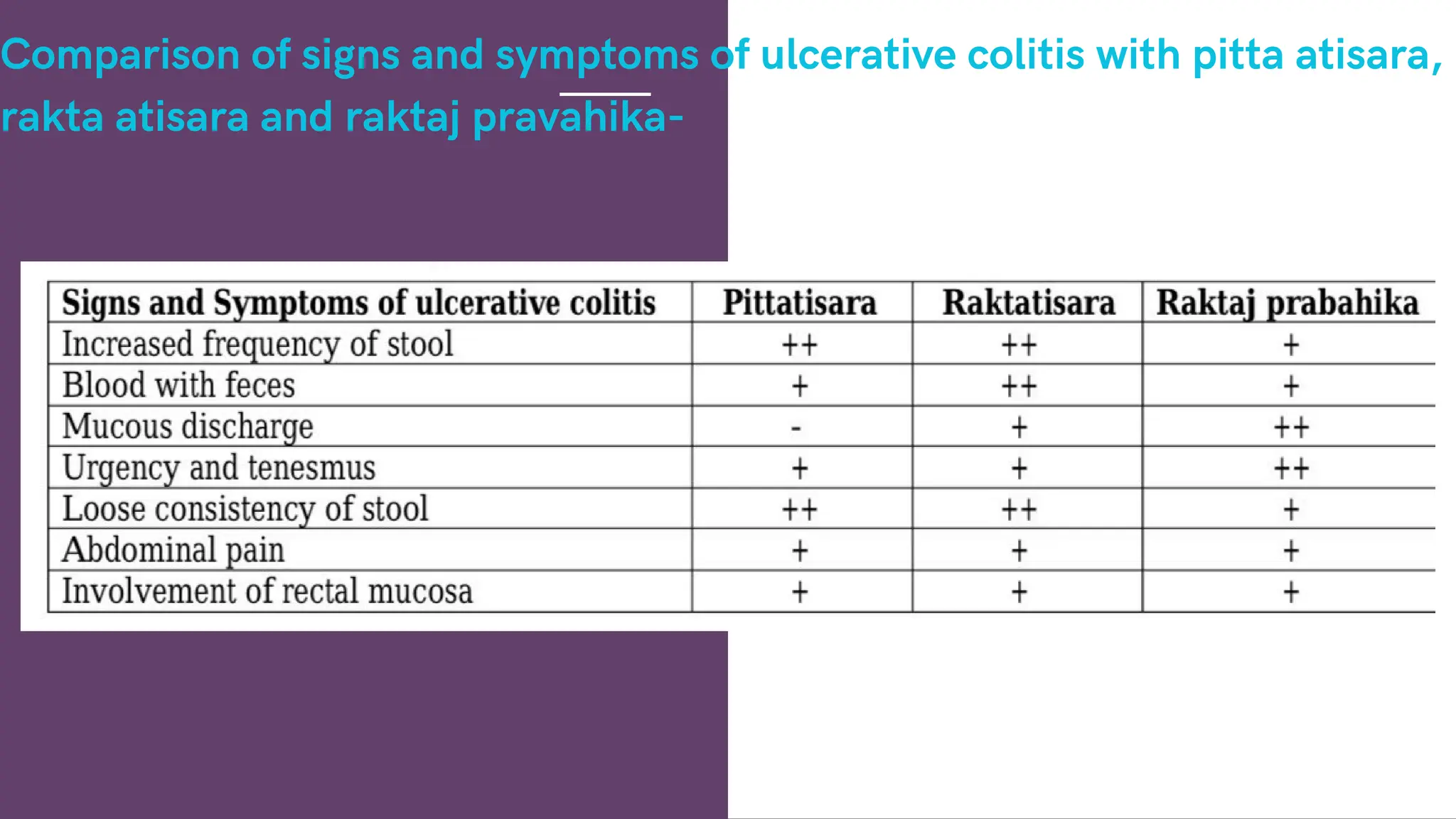
The document discusses the role of Panchakarma in managing ulcerative colitis, an inflammatory bowel disease characterized by chronic inflammation of the colon, and highlights various clinical features and complications. It outlines the pathophysiology, diagnosis, and treatment strategies including lifestyle changes, dietary recommendations, and Ayurvedic therapies, particularly Panchakarma techniques for effective management. Additionally, the document emphasizes the importance of individualized treatment based on patient condition and dosha balance in Ayurveda.