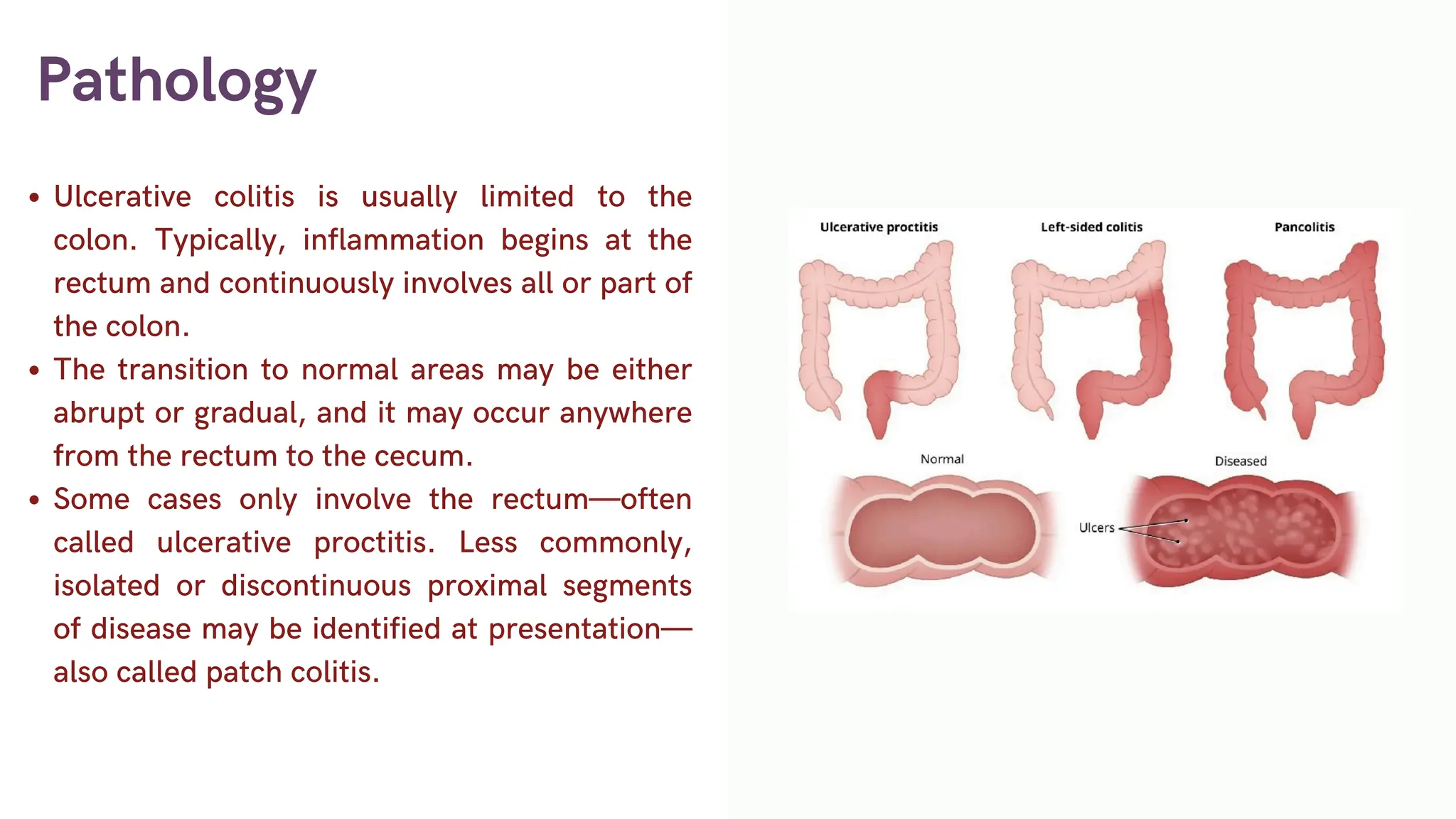
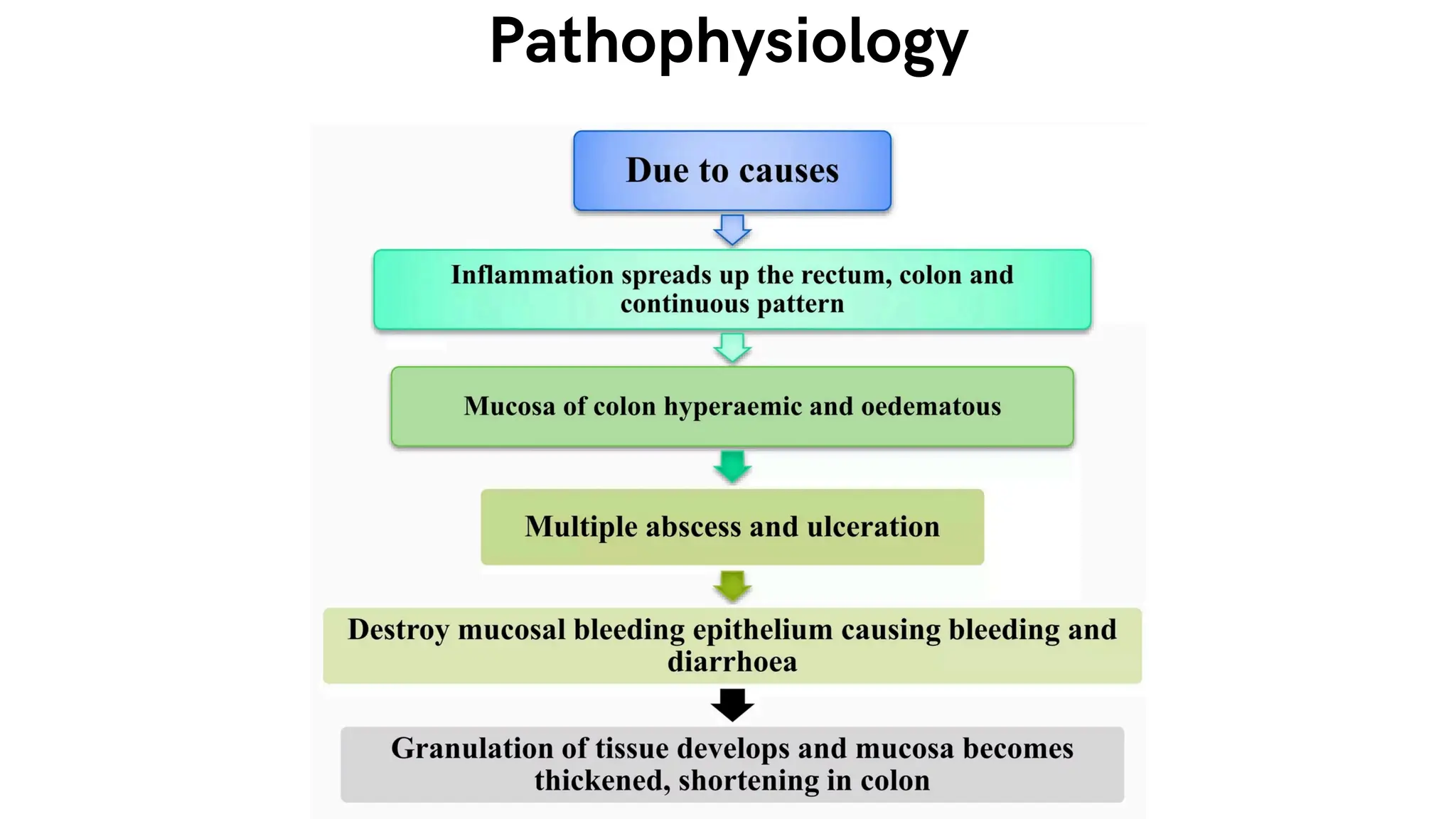
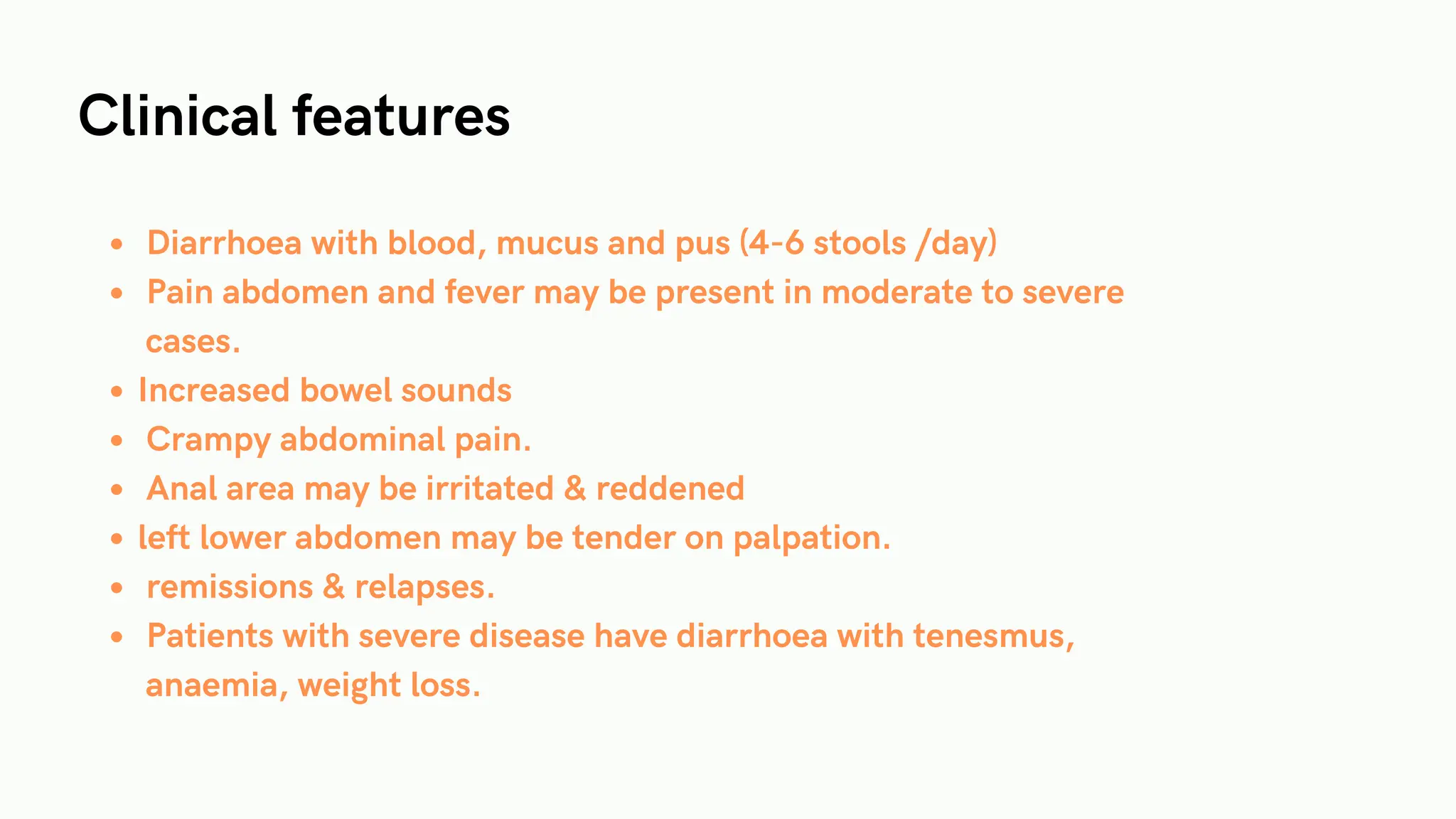
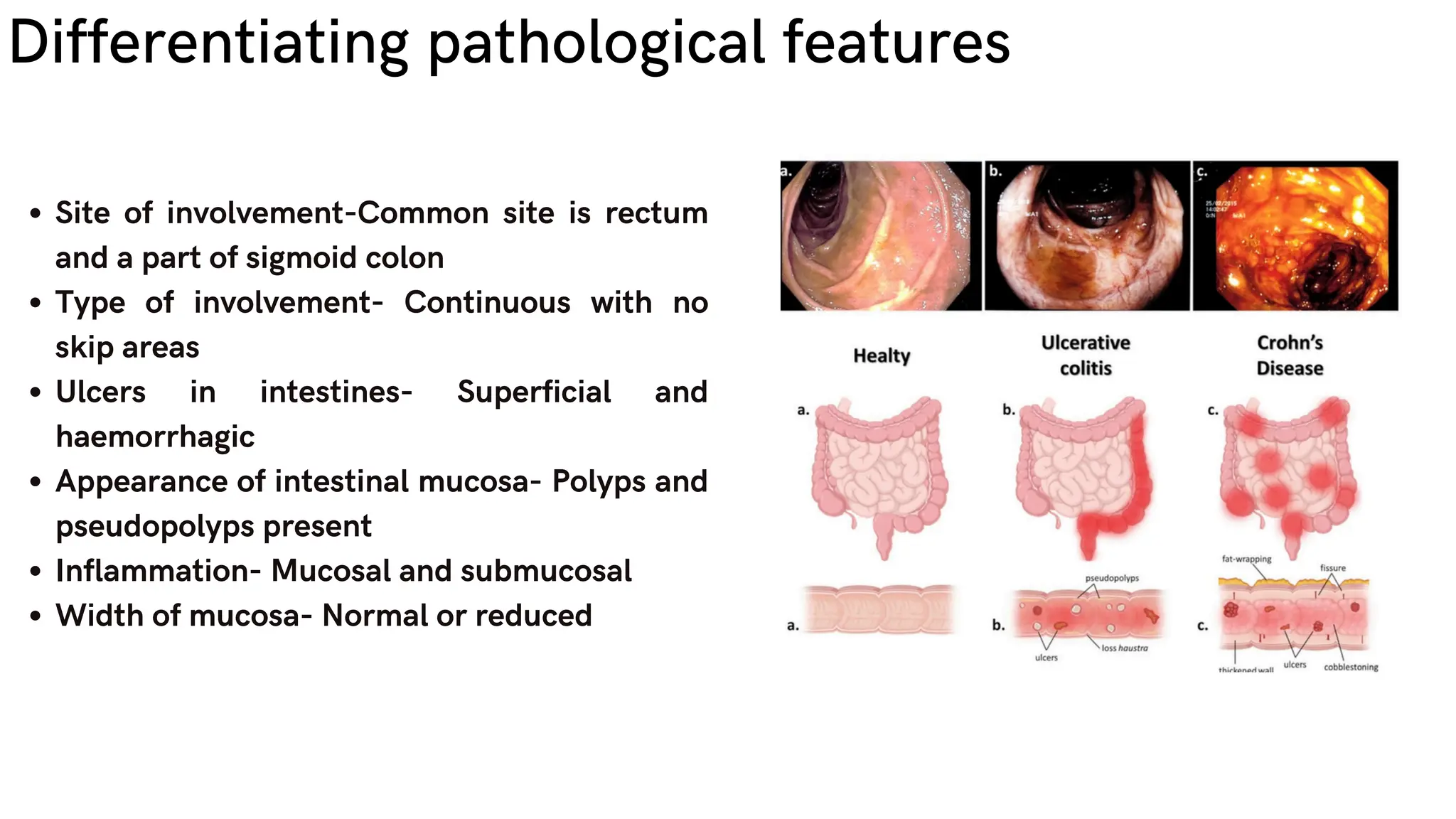
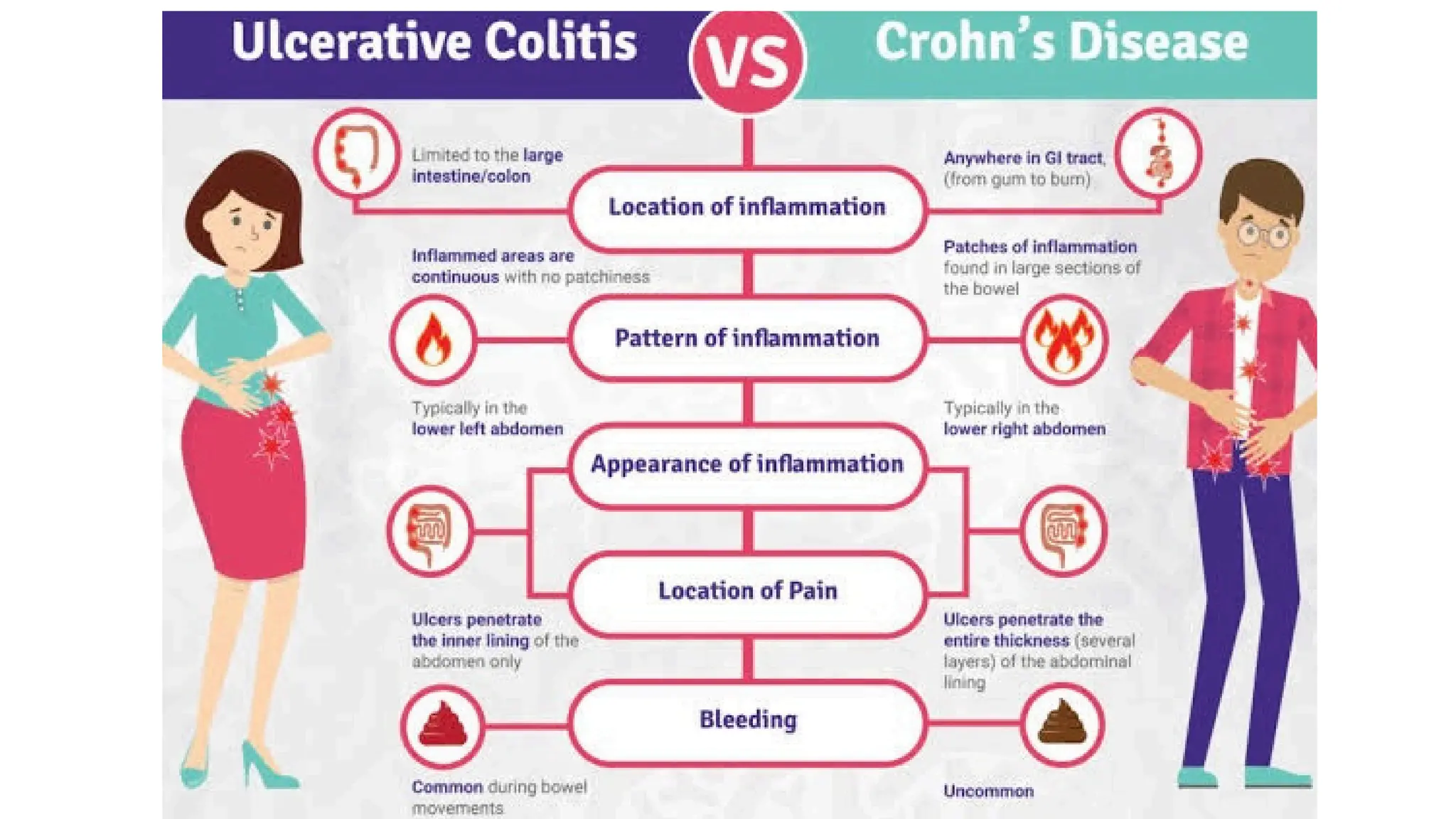
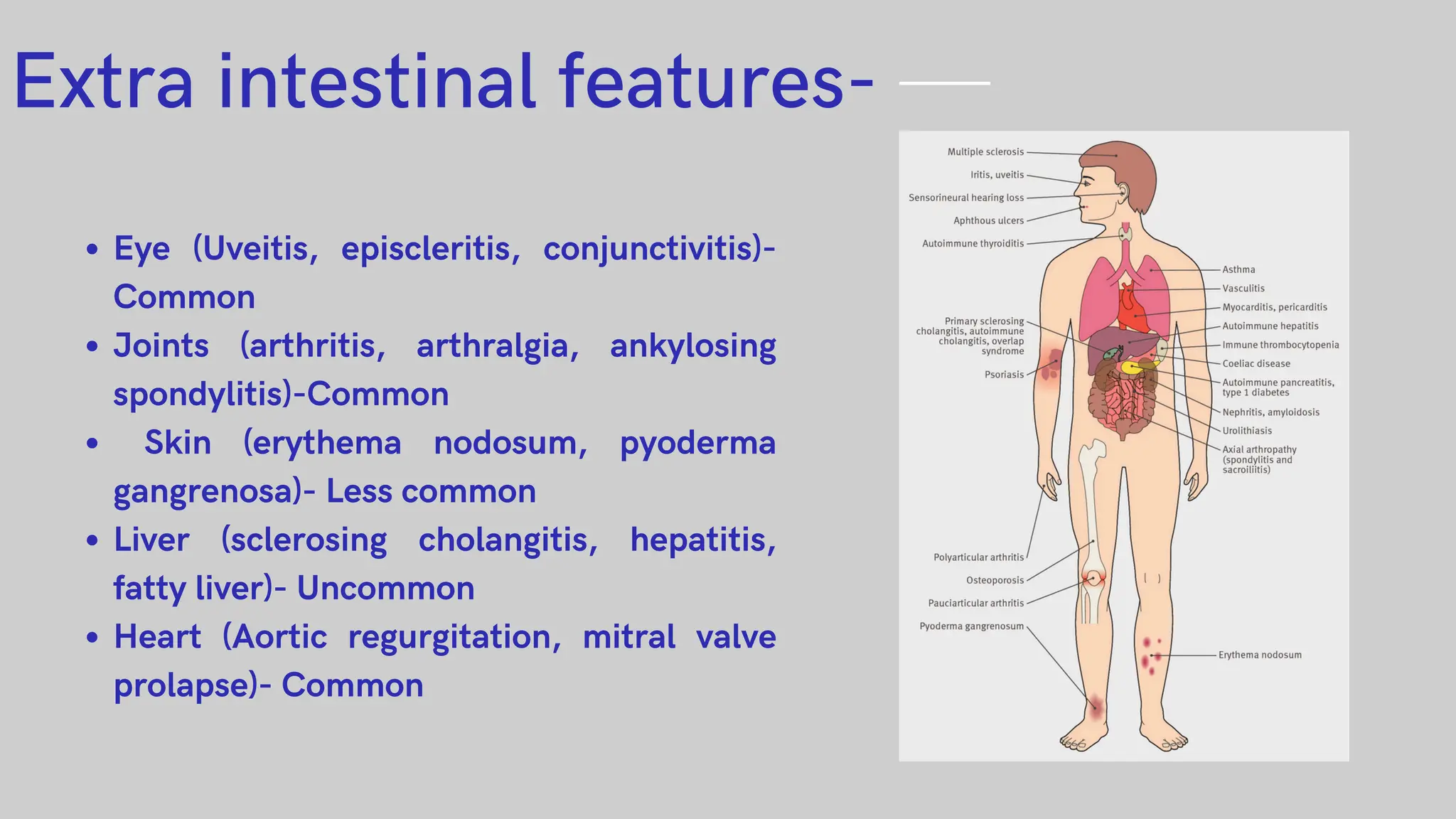
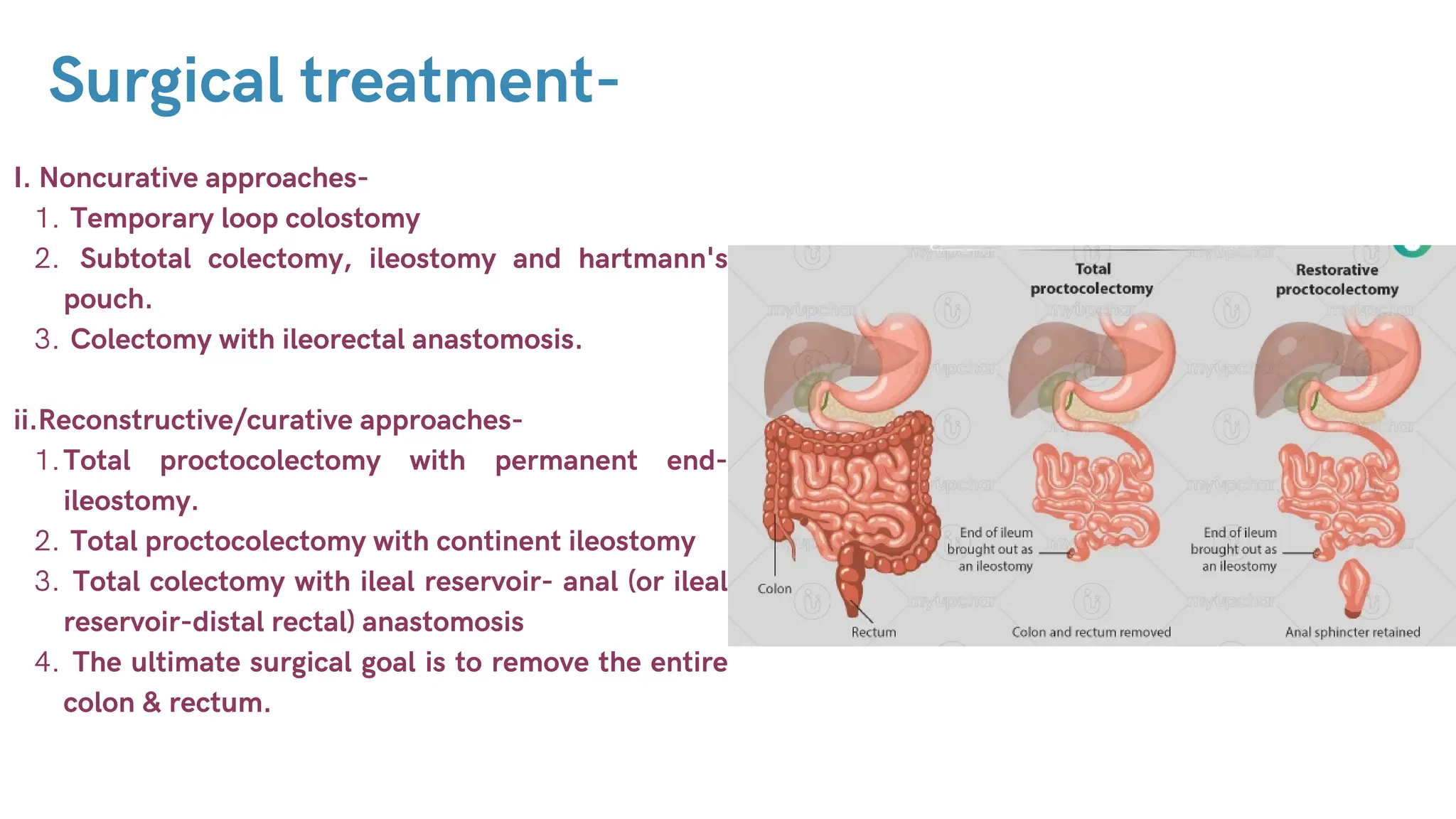
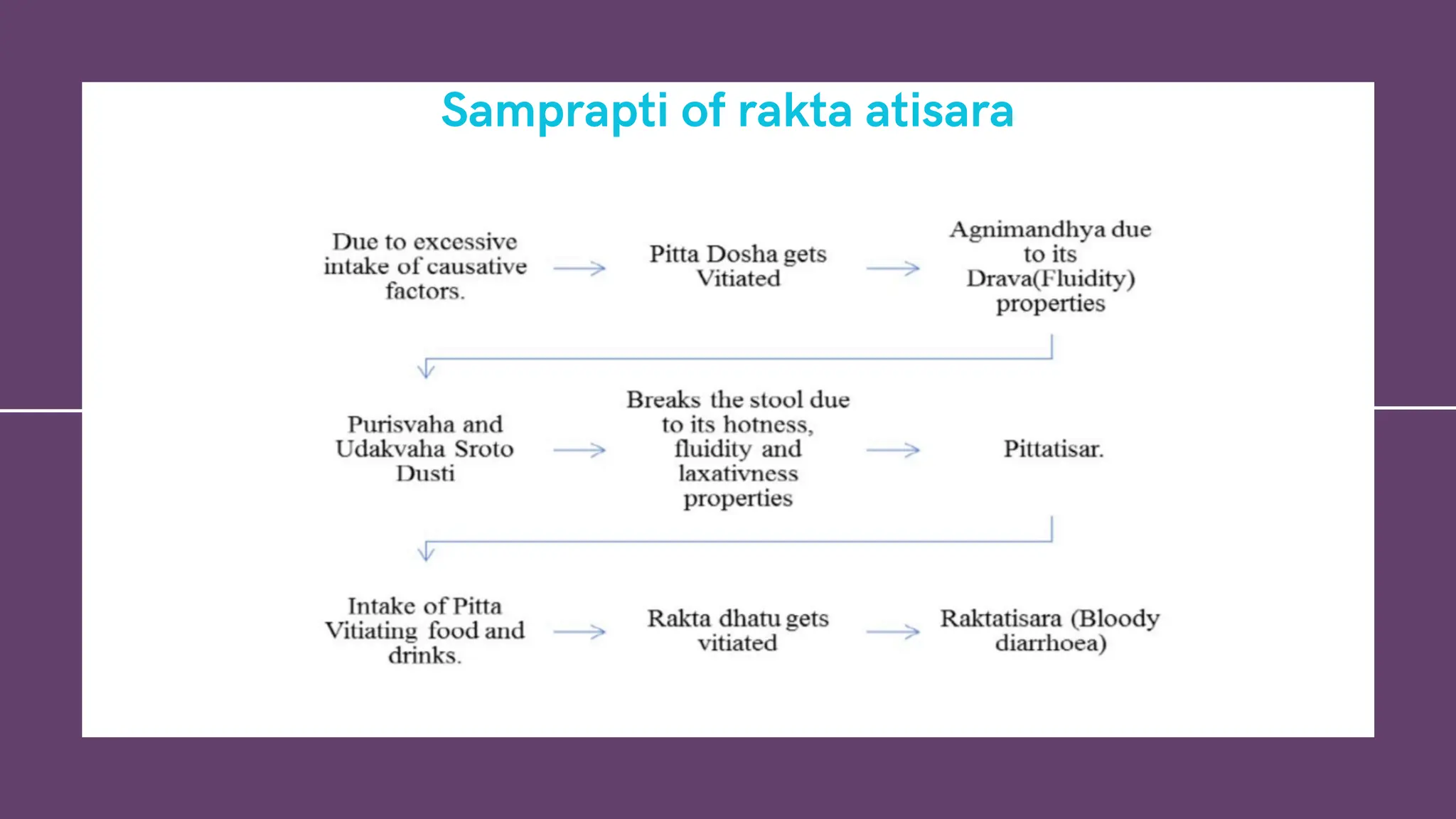
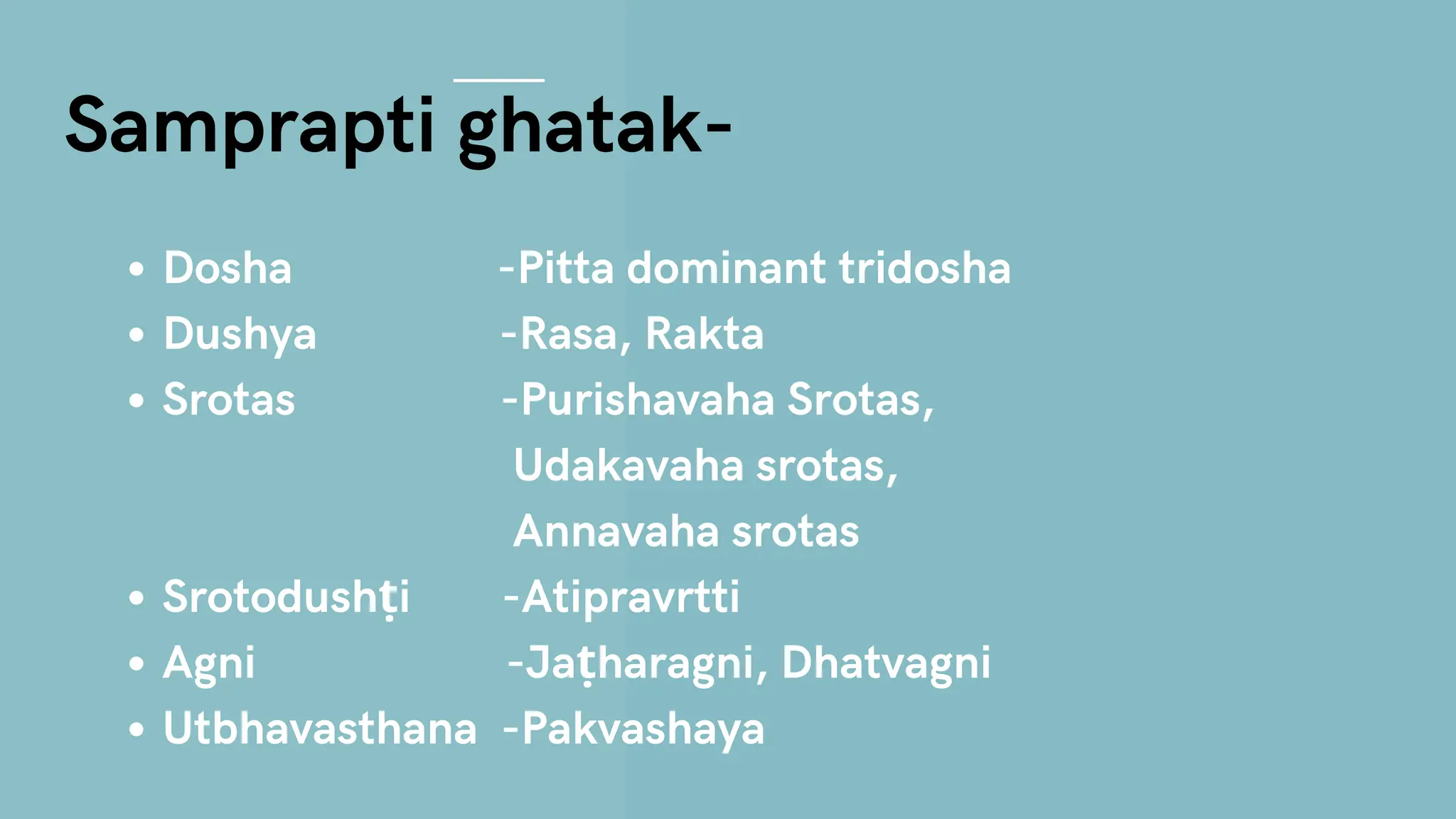
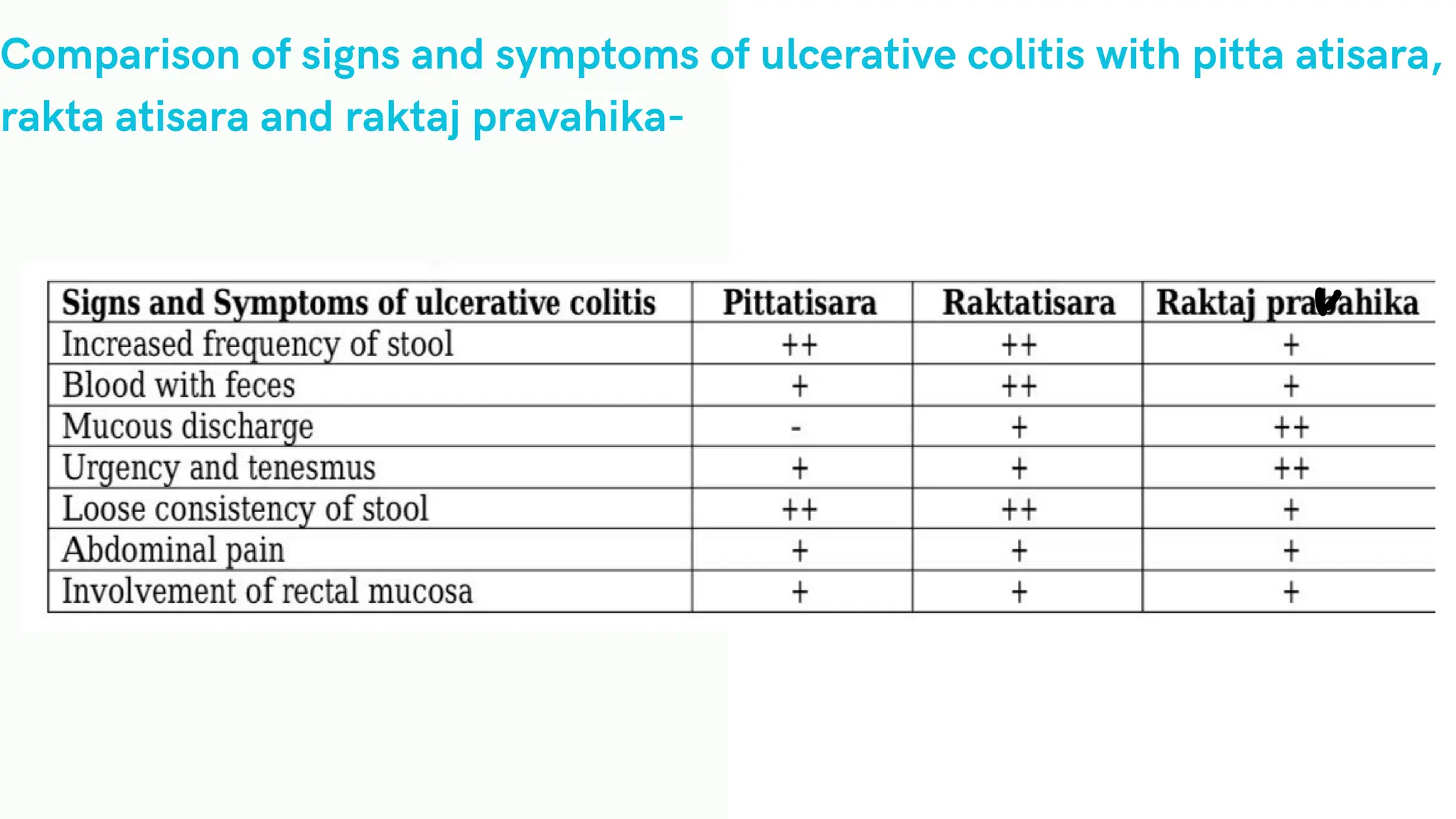
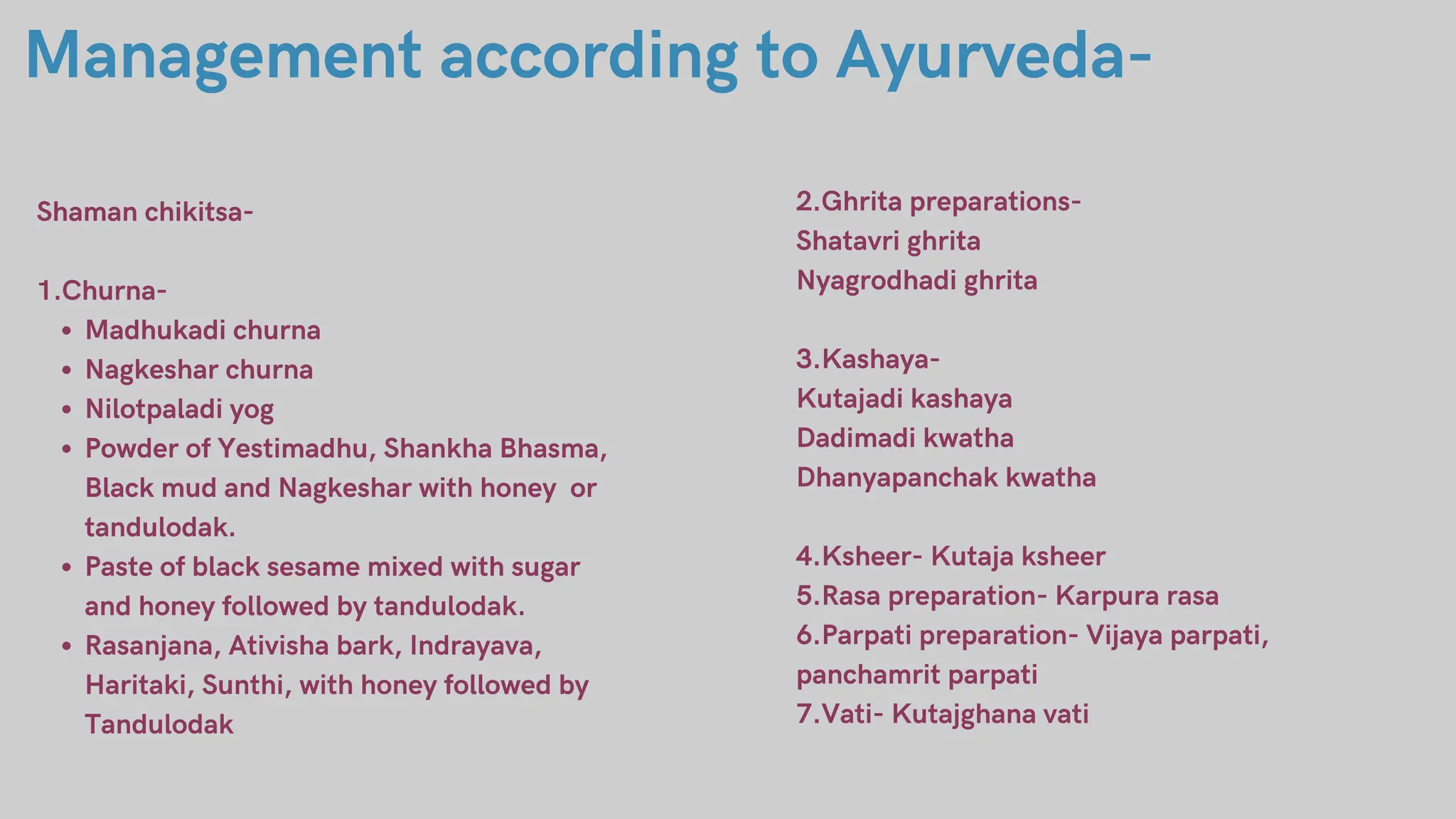
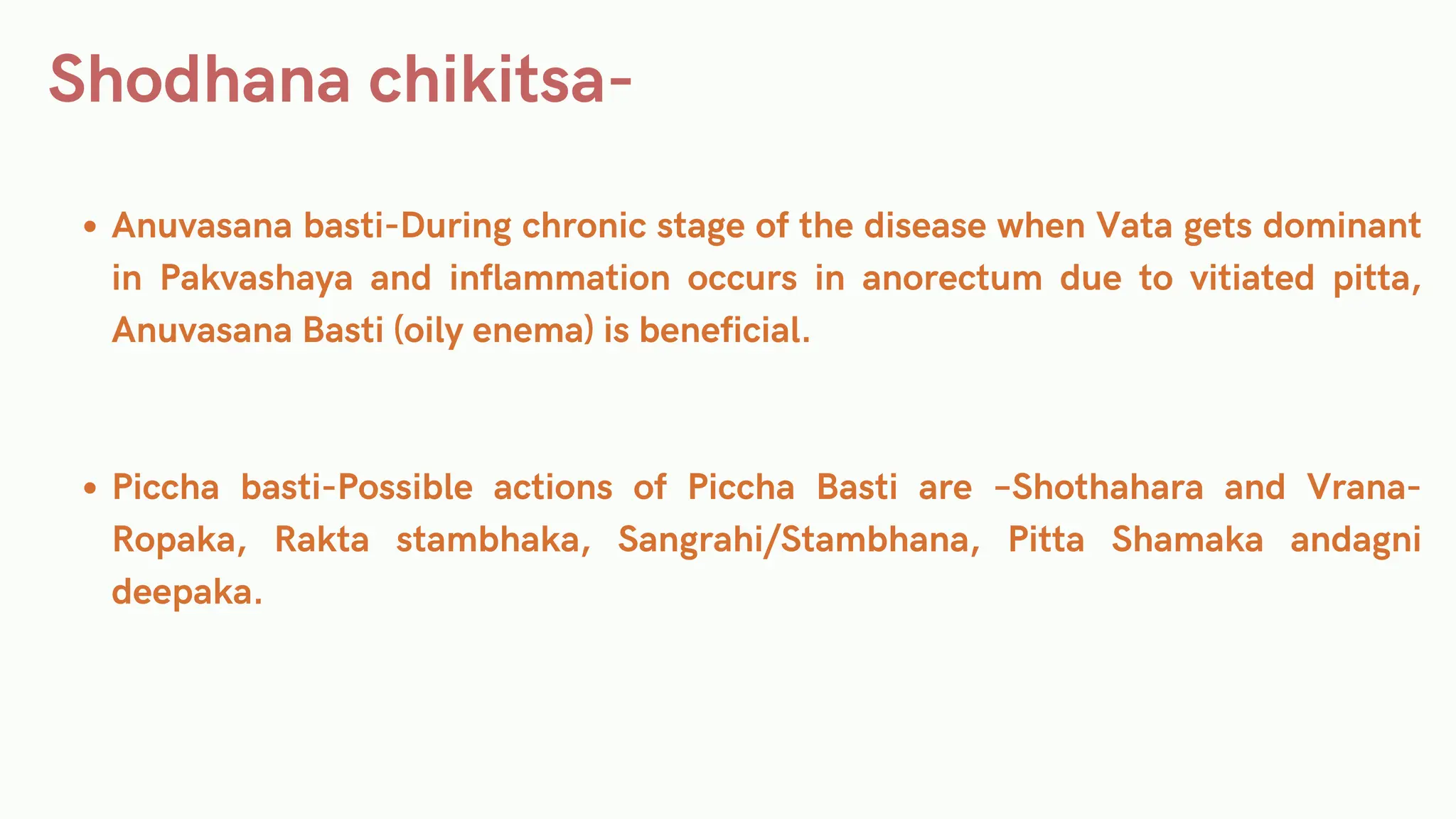
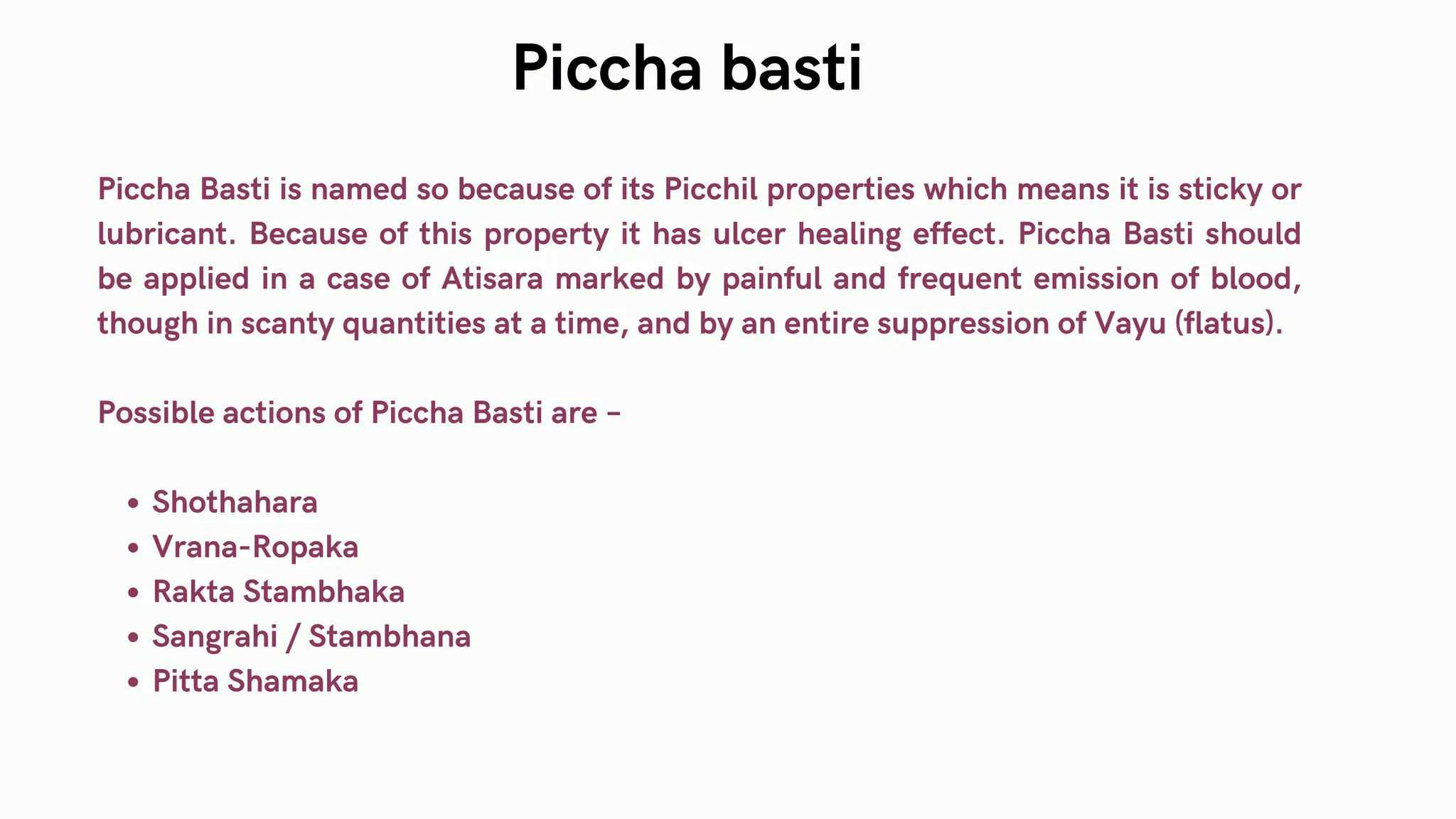
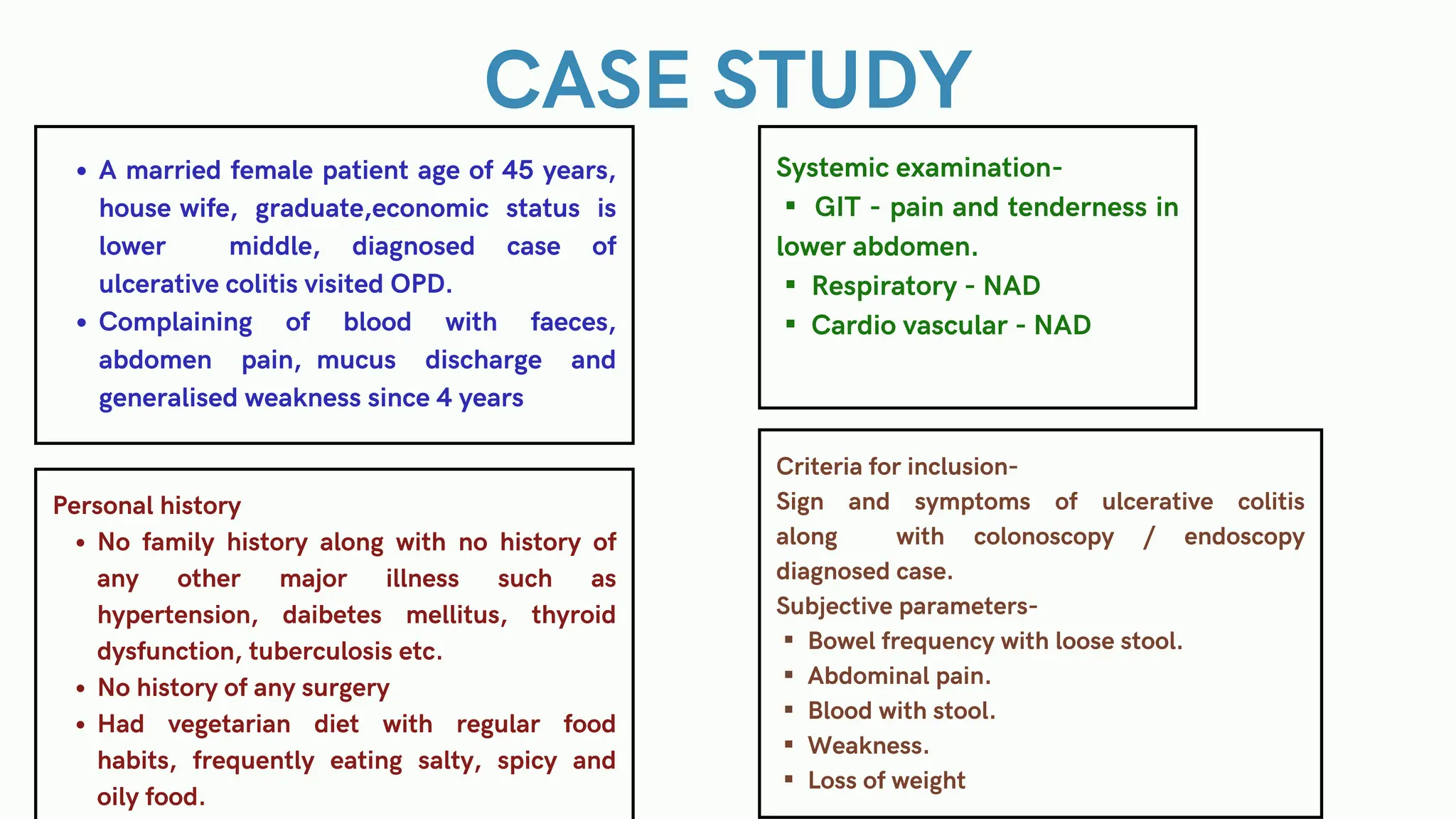
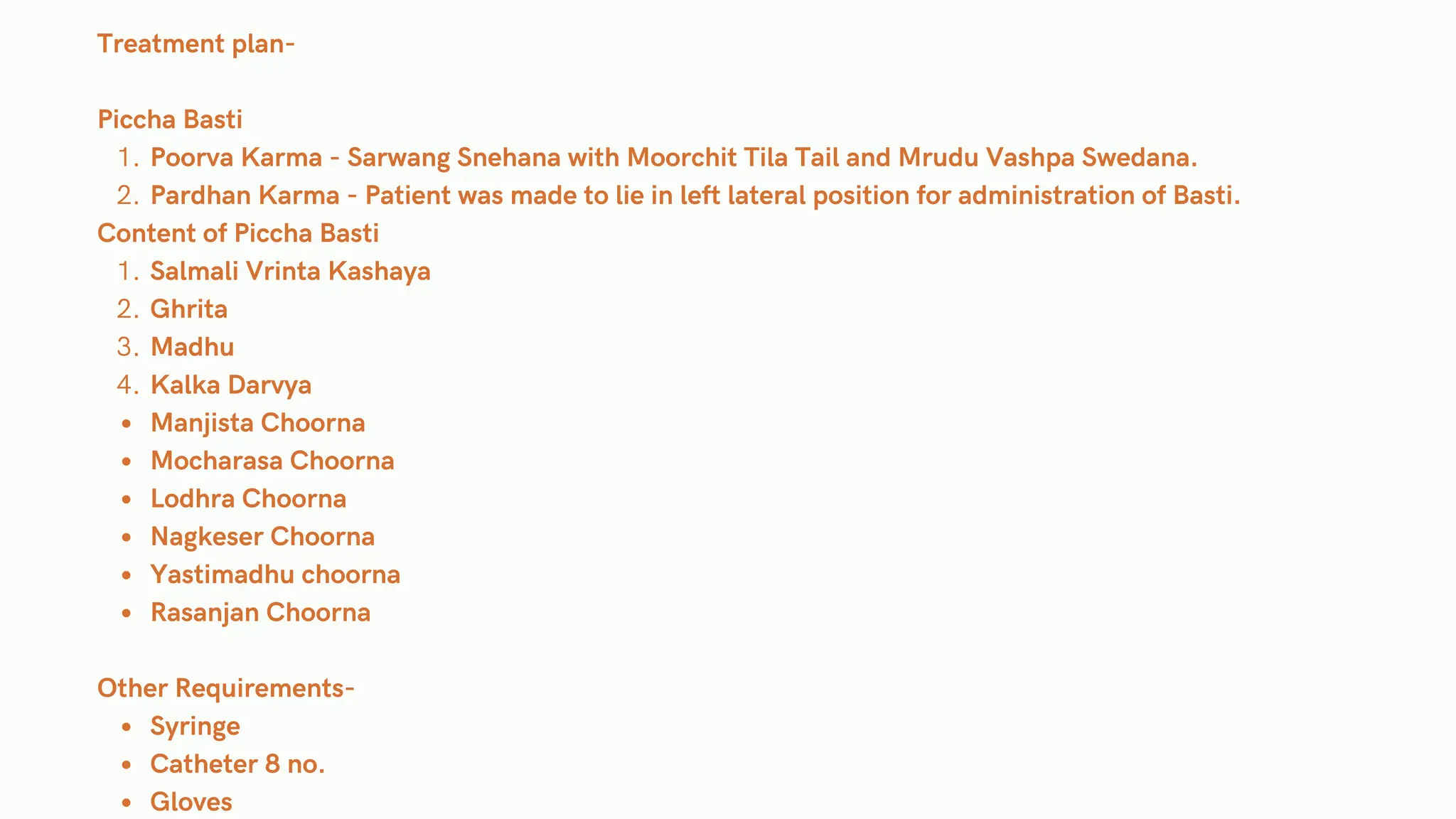
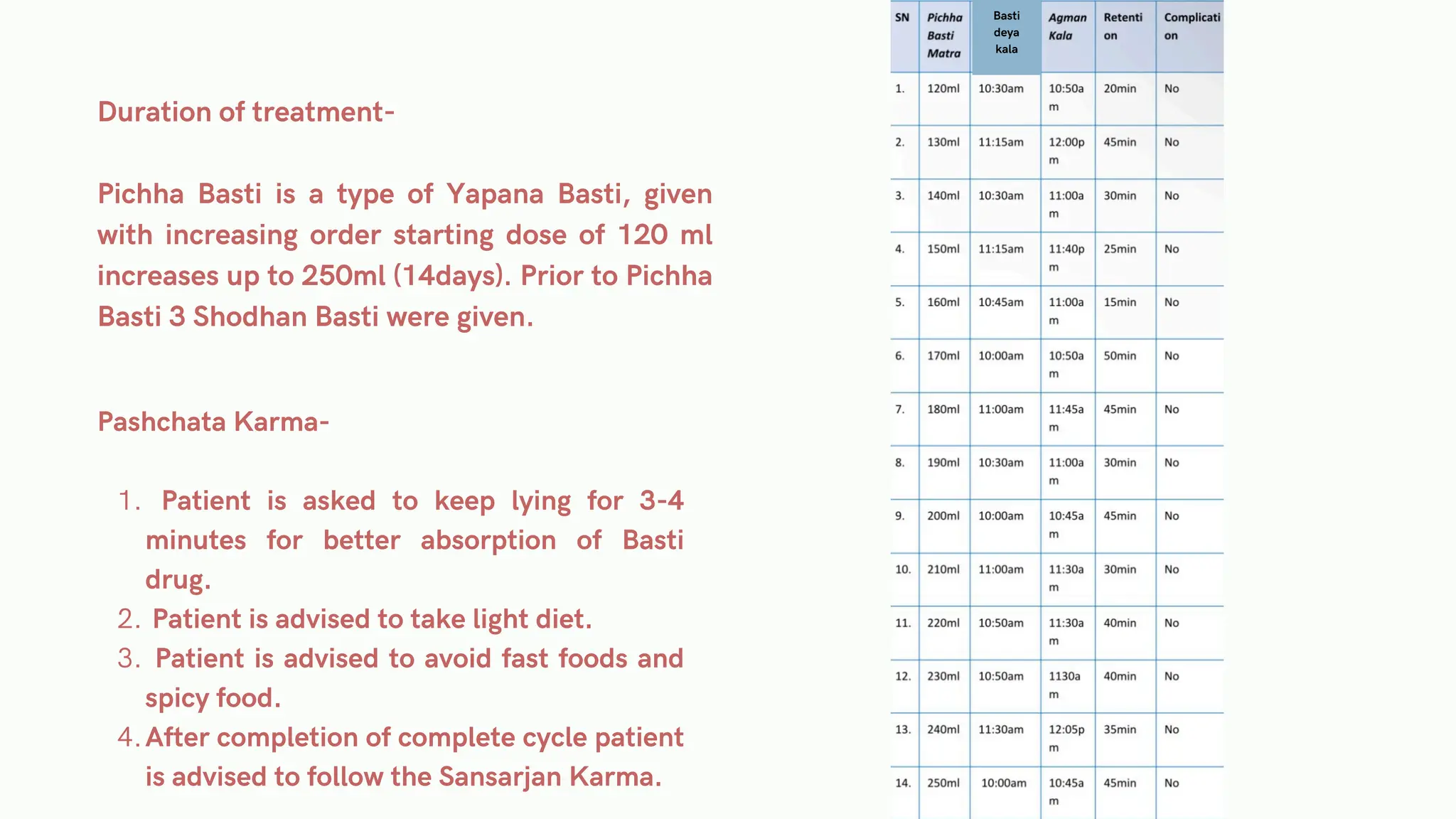
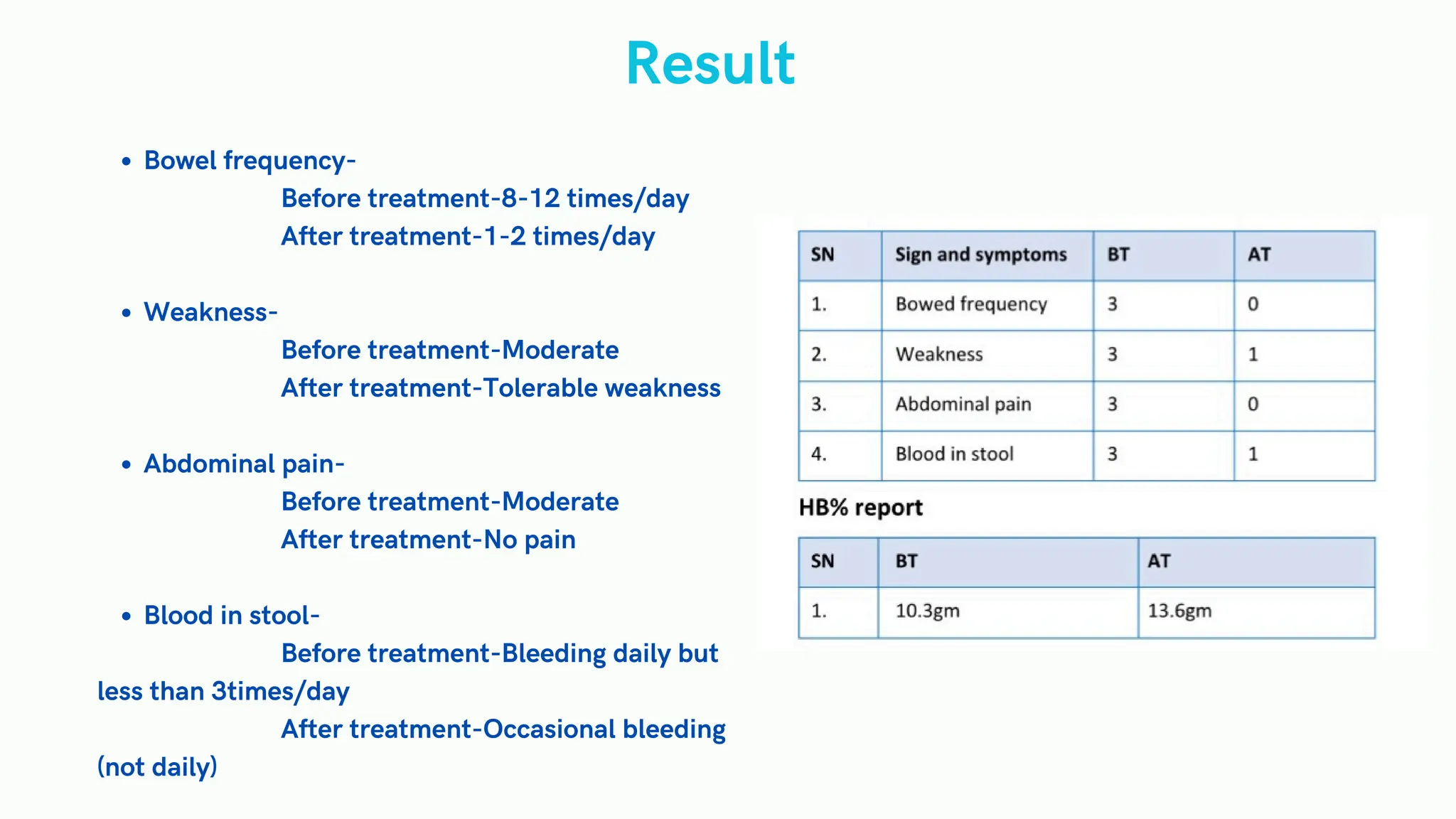
The document discusses ulcerative colitis, a type of inflammatory bowel disease characterized by inflammation of the colon, with varying severity among patients. It covers etiology, pathology, clinical features, diagnosis, and treatment options, including medical management and surgical interventions. The document also explores dietary recommendations and Ayurvedic approaches for managing the disease, supplemented by a case study highlighting treatment outcomes.