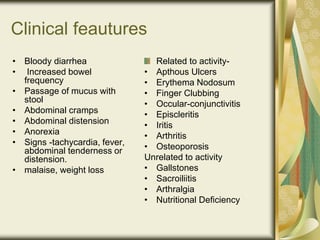
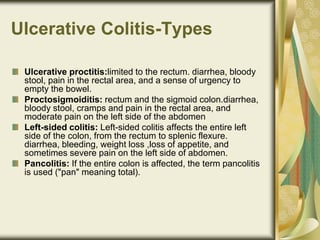
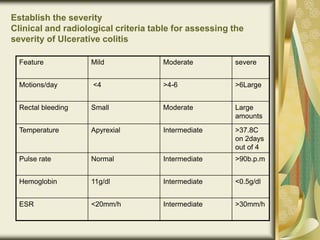
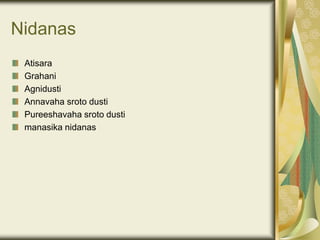
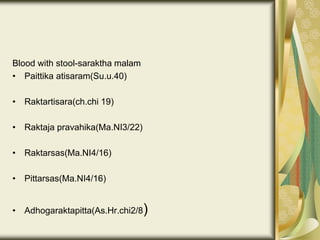
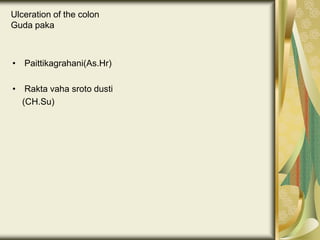
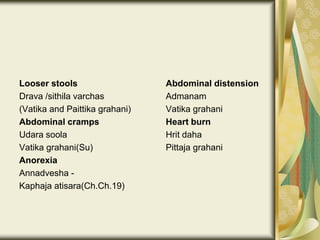
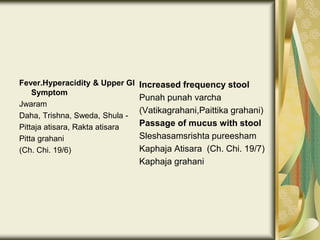
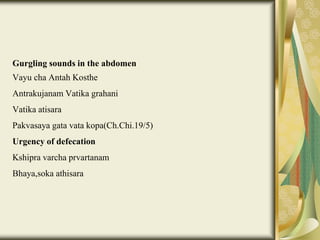
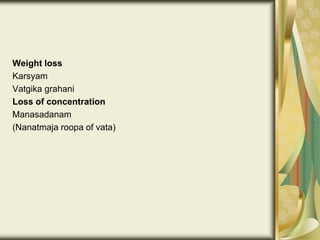
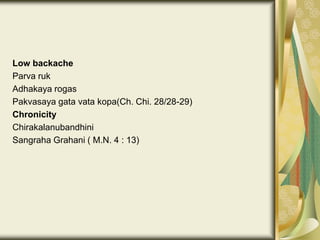
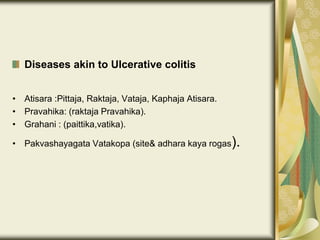
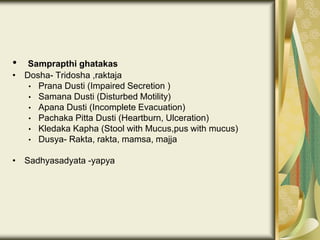
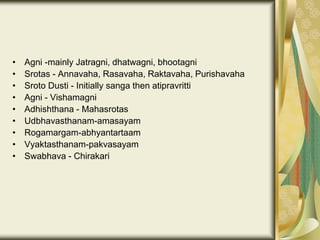
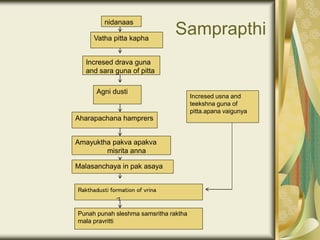
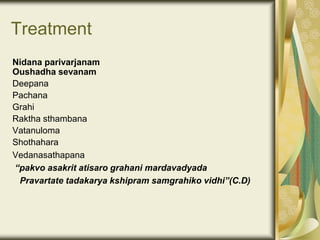
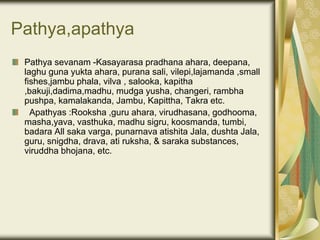
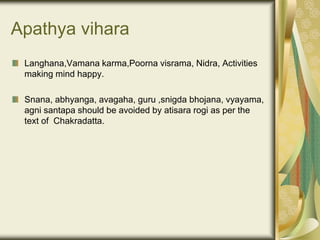
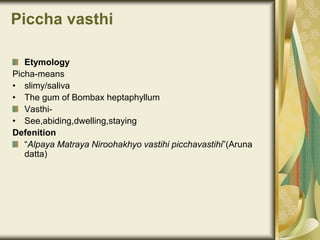
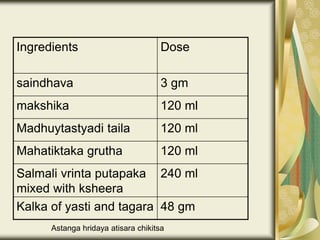
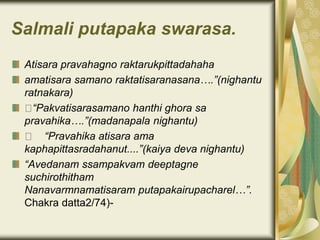
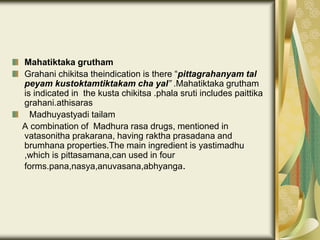
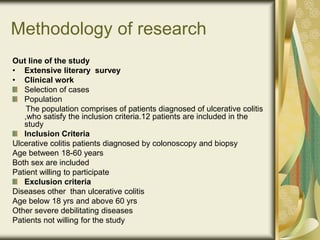
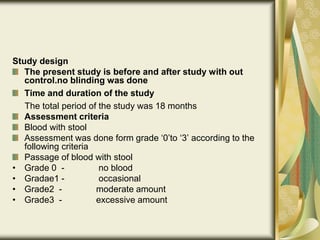
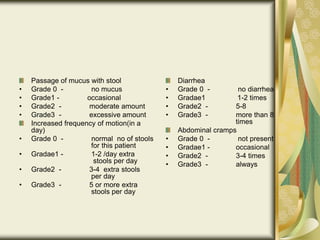
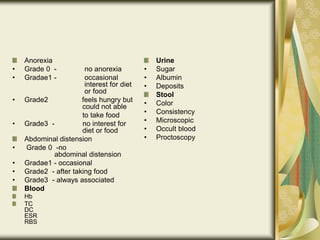
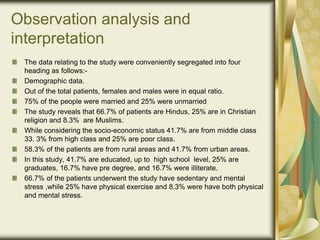
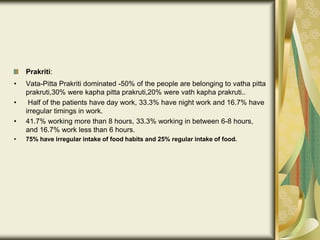
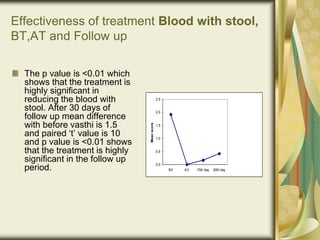
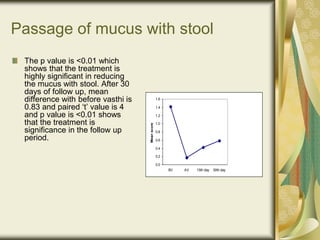
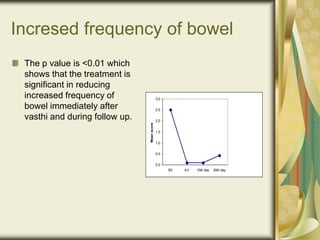
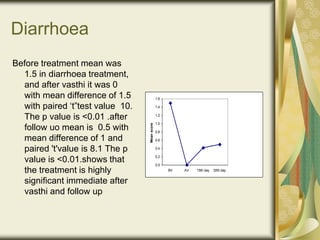
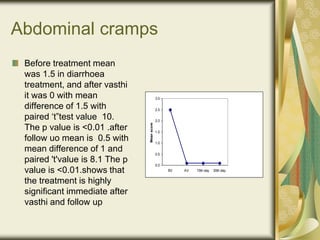
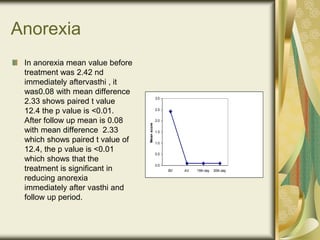
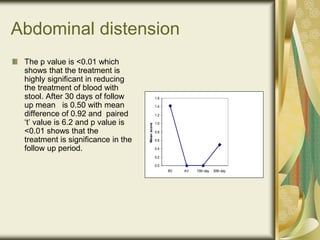
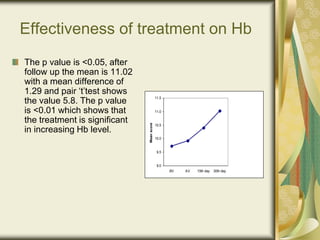
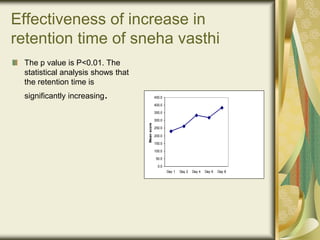
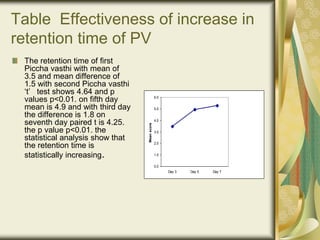
The document outlines a clinical trial to evaluate the efficacy of piccha vasthi in alleviating symptoms of ulcerative colitis, including its definitions, etiology, clinical features, management, and treatment options from both modern and Ayurvedic perspectives. It includes details on the methodology of the research, demographics of participants, assessment criteria, and hypotheses regarding the treatment's significance. The study emphasizes the need for prompt treatment and maintenance in managing ulcerative colitis to prevent relapses.