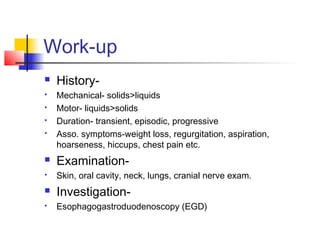
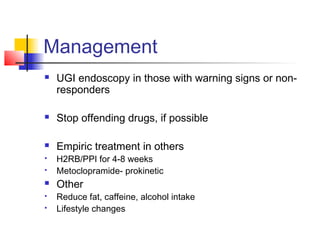
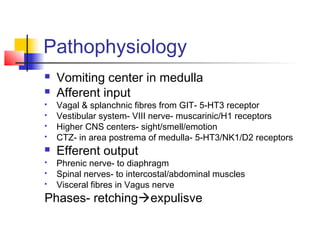
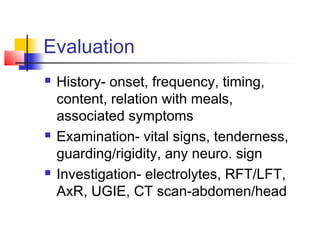
This document discusses upper gastrointestinal (UGI) symptoms including dysphagia, dyspepsia/heartburn, and nausea & vomiting. It provides details on the pathophysiology, causes, evaluation, and treatment of each condition. Dysphagia can be mechanical or motor in origin and caused by issues like esophagitis or achalasia. Dyspepsia is mostly functional but can be due to conditions like GERD. Nausea and vomiting are mediated by brain centers and receptors that can be stimulated by infections, medications, or other visceral issues. Treatment involves addressing the underlying cause, rehydration, and antiemetics as appropriate for the condition.