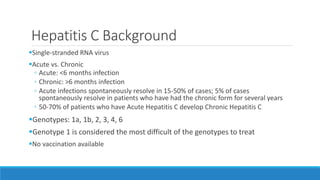
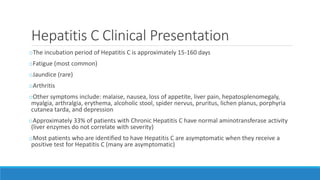
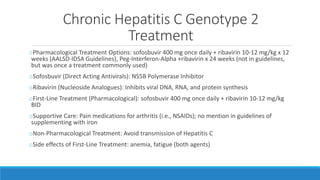
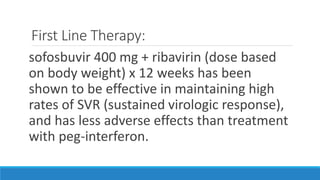
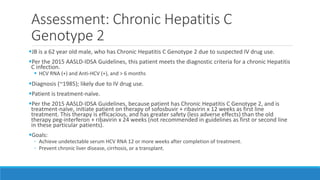
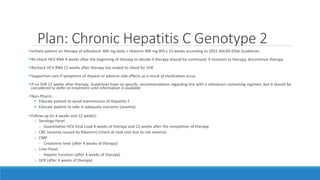
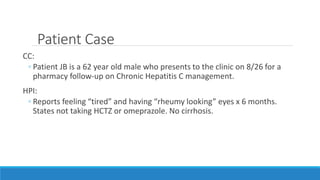
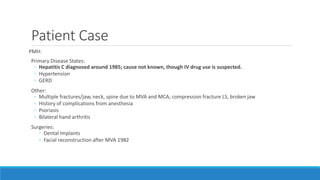
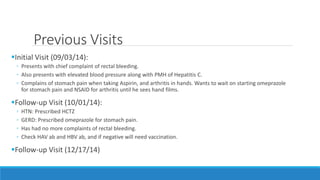
This patient has chronic hepatitis C genotype 2 infection, hypertension, and GERD. He has fatigue and eye symptoms and a history of IV drug use suspected as the cause of his hepatitis C infection. His hepatitis C viral load is elevated and he has no cirrhosis. Treatment with 12 weeks of sofosbuvir and ribavirin is planned to achieve sustained virologic response and prevent progression of liver disease. His hypertension is also being monitored and managed.
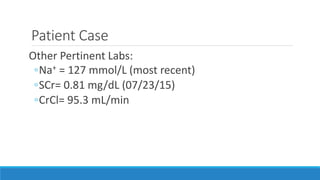
![Patient Case
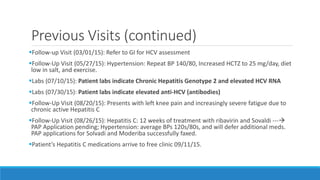
Physical Exam:
Vitals: (8/26/15)
◦ Wt: 194.0 lbs. (88kg)
◦ Ht/Lt in: 70.0’’
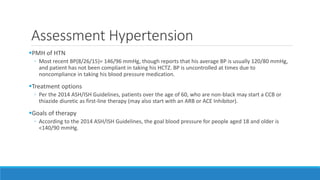
◦ BP: 146/96 mmHg
◦ Pulse: 60 bpm
◦ BMI: 27.8 kg/m2
Pertinent Labs:
• HCV Fibrosure: 0.98 (07/30/15)
• Hep C Virus Ab > 11.0 [IU]/mL (07/30/15)
• Hep C Quantity (A) 3,802,150 [IU]/mL
( 07/10/15)
• Genotype 2 (07/10/15)
• HIV: Negative (09/03/14)
• RA Latex Turbid= 90.8 [IU]/mL (06/04/15)
• ALT= 414 U/L (07/30/15)
• AST= 196 U/L (07/23/15)
• Haptoglobin <10 mg/dL (07/30/15)](https://image.slidesharecdn.com/c6503476-bfba-45d6-b61e-d607b9df9b37-161226054634/85/Hepatitis-C-Presentation-10-320.jpg)