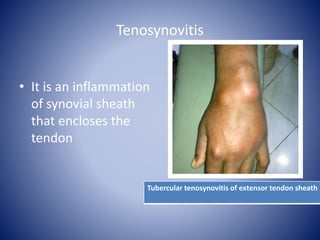
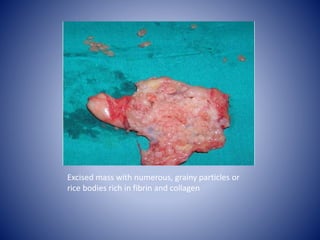
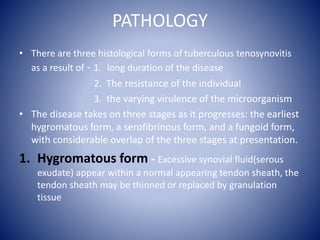
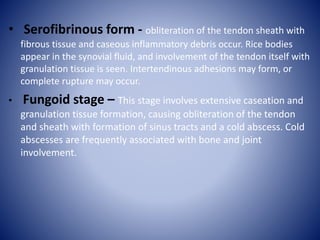
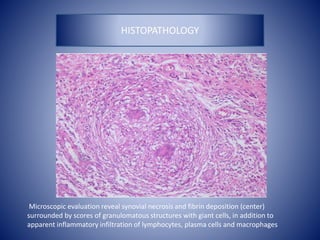
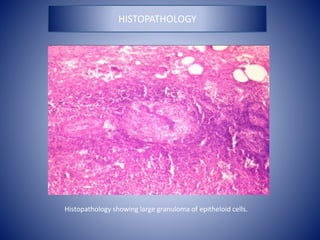
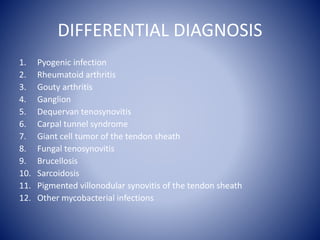
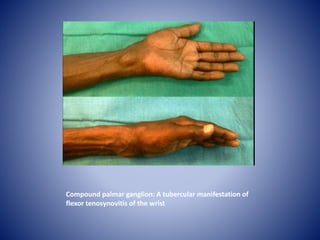
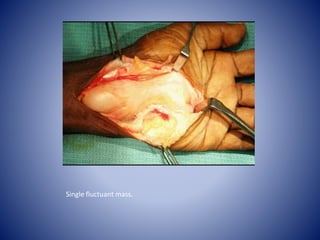
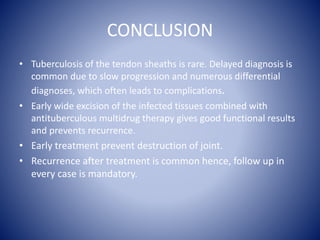
Tuberculous tenosynovitis, or tuberculosis of the tendon sheaths, is a rare form of extrapulmonary tuberculosis that can lead to complications if not properly diagnosed and treated. It occurs when tuberculosis bacteria infect the synovial sheaths surrounding tendons. On histopathological examination, rice bodies may be seen within the synovial fluid. Treatment involves immobilizing the affected area, administering antitubercular drugs for 9-12 months, and potentially surgical debridement if symptoms persist or worsen. Early diagnosis and treatment can prevent joint destruction and recurrence of symptoms.