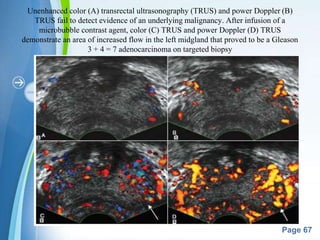
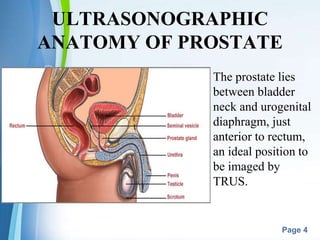
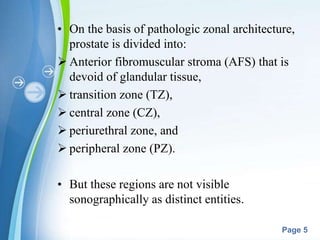
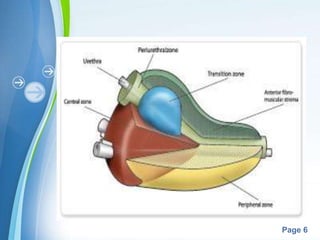
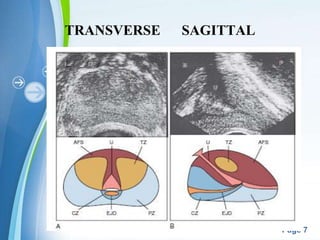
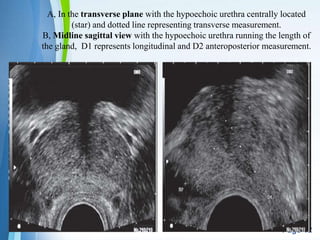
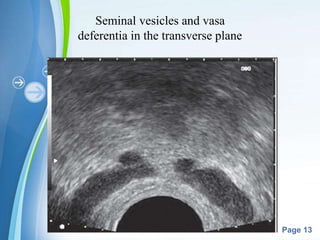
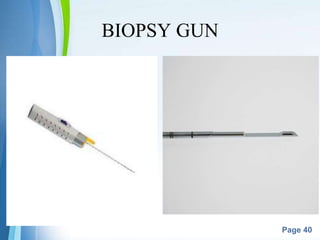
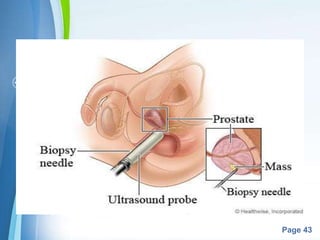
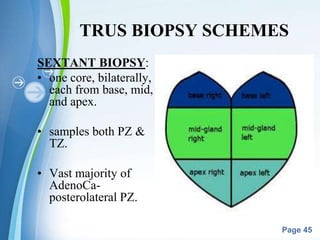
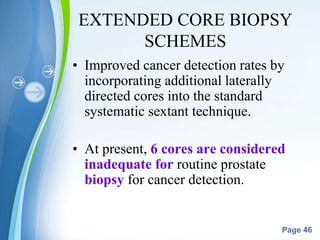
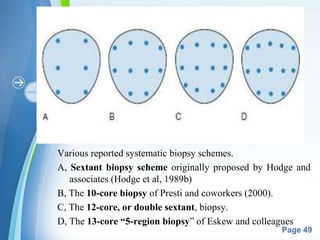
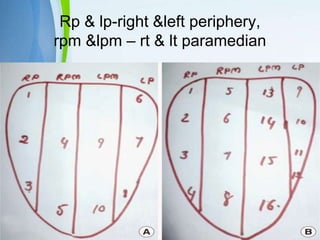
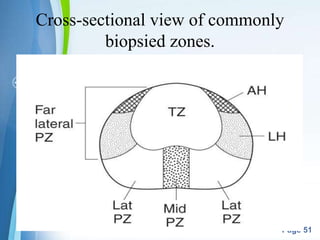
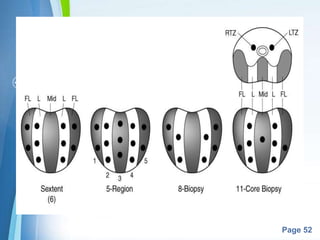
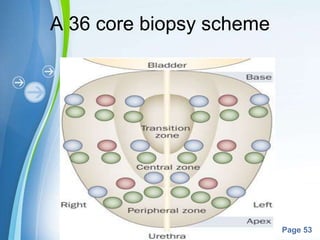
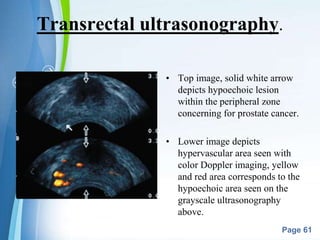
This document describes transrectal ultrasound (TRUS)-guided prostate biopsy techniques. It begins with background on the anatomy of the prostate and ultrasonographic imaging. TRUS-guided biopsy is considered the mainstay for prostate cancer detection and involves using a biopsy gun to obtain core samples under ultrasound guidance. Various biopsy schemes are described, including the original sextant technique and more extensive schemes involving additional cores. Factors such as patient preparation, anesthesia, and antibiotic prophylaxis for biopsies are also outlined. The document provides an overview of TRUS-guided prostate biopsy procedures and technical considerations.



![Powerpoint Templates
Page 62
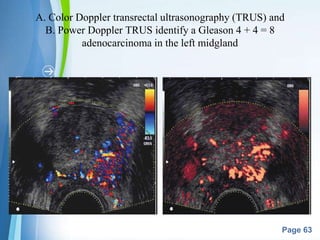
POWER DOPPLER IMAGING (enhanced color
Doppler, color amplitude imaging [CAI], or
color angiography) uses amplitude shift to
detect flow in a velocity and directionally
independent manner.
• Advantages: ability to detect slower flow and
to have less reliance on the Doppler angle,
making it more suitable for detection of
prostate cancer neovascularity.](https://image.slidesharecdn.com/trusbiopsyprostate-151226120433/85/Trus-biopsy-prostate-62-320.jpg)