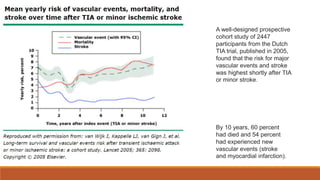
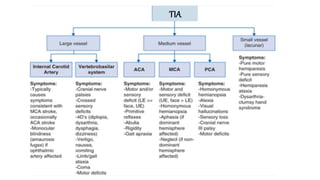
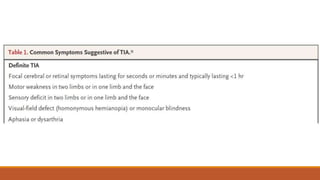
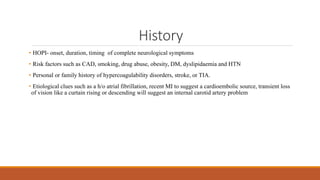
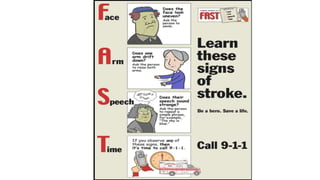
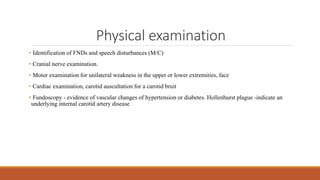
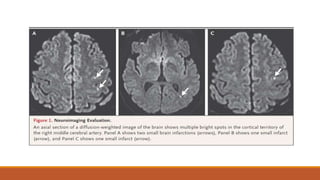
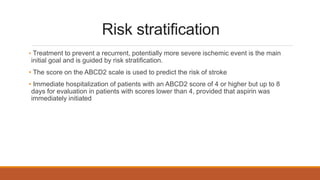
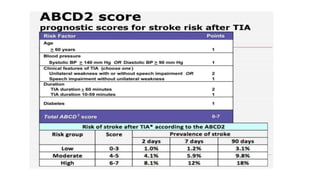
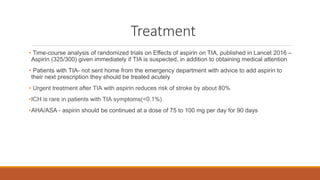
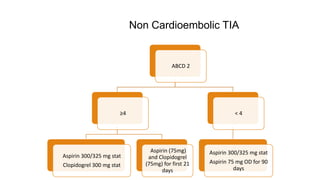
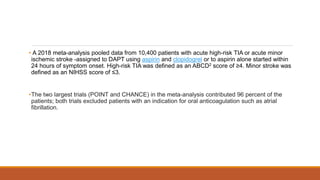
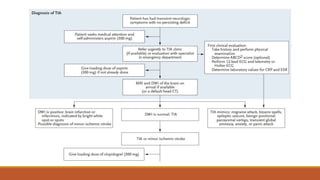
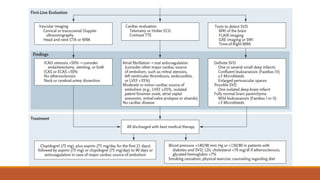
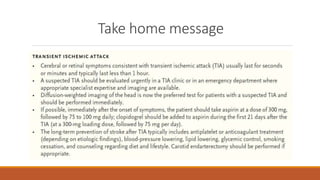
A 54-year-old man presented with transient left arm weakness. He has risk factors including hypertension, hyperlipidemia, and smoking. Evaluation of transient ischemic attack (TIA) includes diffusion-weighted MRI, carotid imaging, ECG, and treating the underlying cause. For this patient, administer aspirin and clopidogrel based on his high ABCD2 score, and consider carotid endarterectomy if significant stenosis is found to prevent recurrent stroke. Long-term management focuses on risk factor control through medication and lifestyle changes.