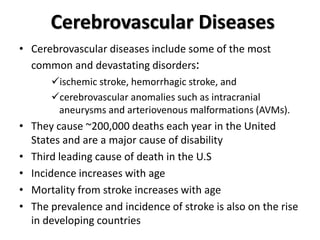
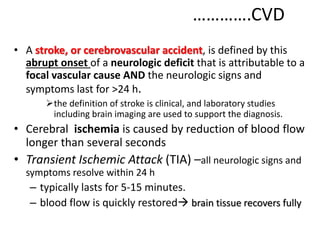
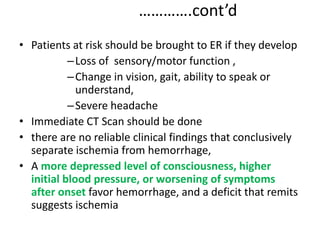
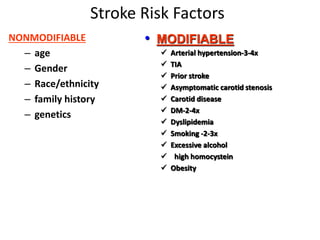
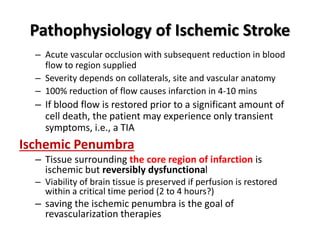
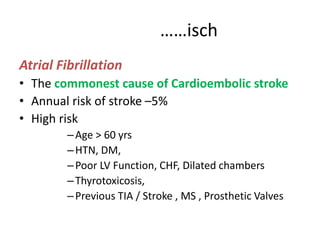
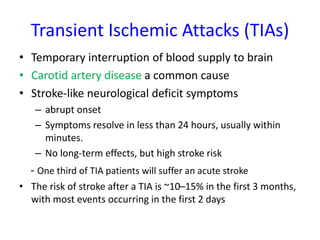
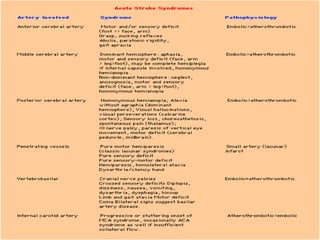
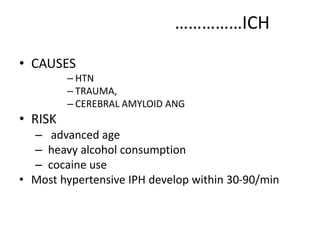
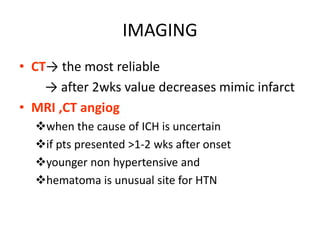
Cerebrovascular diseases like stroke are a major cause of death and disability in the US. There are two main types of stroke - ischemic caused by blockage of an artery and hemorrhagic caused by bleeding. Risk factors include age, hypertension, diabetes, smoking, prior stroke or TIA. Diagnosis involves brain imaging like CT or MRI. Treatment depends on type and severity but may include thrombolysis, anticoagulation, antiplatelet drugs, managing risk factors, and rehabilitation. Preventing stroke requires risk factor modification and treatments like antiplatelet drugs.