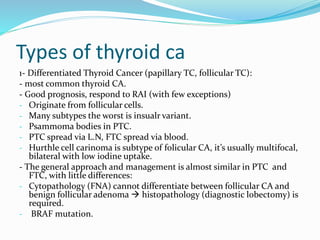
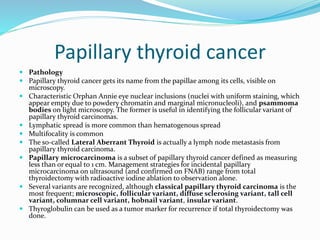
The document provides a comprehensive overview of thyroid nodule management, including surgical anatomy, types of thyroid cancer, diagnostic approaches, and treatment options. It details the surgical procedures involved in thyroidectomies, complications, and the necessary preoperative assessments, emphasizing the roles of ultrasound and fine needle aspiration. Additionally, it covers the prognosis and categorization of different thyroid cancers, highlighting the importance of tailored surgical approaches based on specific conditions.