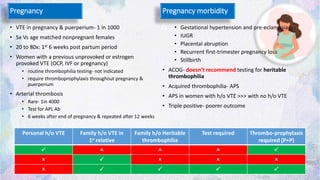
The document discusses thrombophilia testing, outlining who should be tested, when, why, and what to test for, focusing on various inherited and acquired conditions that increase thrombotic risk. It emphasizes the importance of understanding individual patient factors, such as age and family history, in determining the need for testing and management strategies. Additionally, it highlights cases to illustrate the complexity of thrombophilia and provides guidelines on testing and treatment based on the latest research.