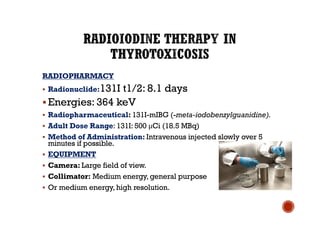
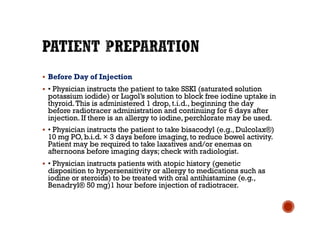
The document discusses radiopharmaceuticals used in nuclear medicine, including 131I and 131I-mIBG. 131I is commonly used to treat thyroid abnormalities like residual thyroid tissue or cancer through oral administration. It has a half-life of 8 days and emits gamma rays and beta particles. 131I-mIBG is used intravenously to detect and treat neuroendocrine tumors through uptake in adrenergic neurons. Proper patient preparation and precautions are needed when administering radiopharmaceuticals to localize and treat various cancer types and reduce radiation exposure. Nuclear medicine procedures can help diagnose and treat conditions like pheochromocytomas, paragangliomas, carcinoid tumors, and neuroblast









![§ [standing] hypotension).These occur within the adrenal
medulla and are frequently associated
§ with hereditary multiple endocrine neoplasia (MEN)
types 2A and 2B, neurofibromatosis, von
§ Hippel-Lindau disease, Carney’s triad, and familial
pheochromocytoma.
§ • Localization of site(s) of hormonal overproduction.
§ • Detection and localization of neuroectodermal (nerve
tissue) tumors.
§ • Paragangliomas (tumors of the adrenal medulla,
chromaffin cells, and the paraganglia)](https://image.slidesharecdn.com/therapeuticapplication1-200516140413/85/Therapeutic-application-14-320.jpg)






