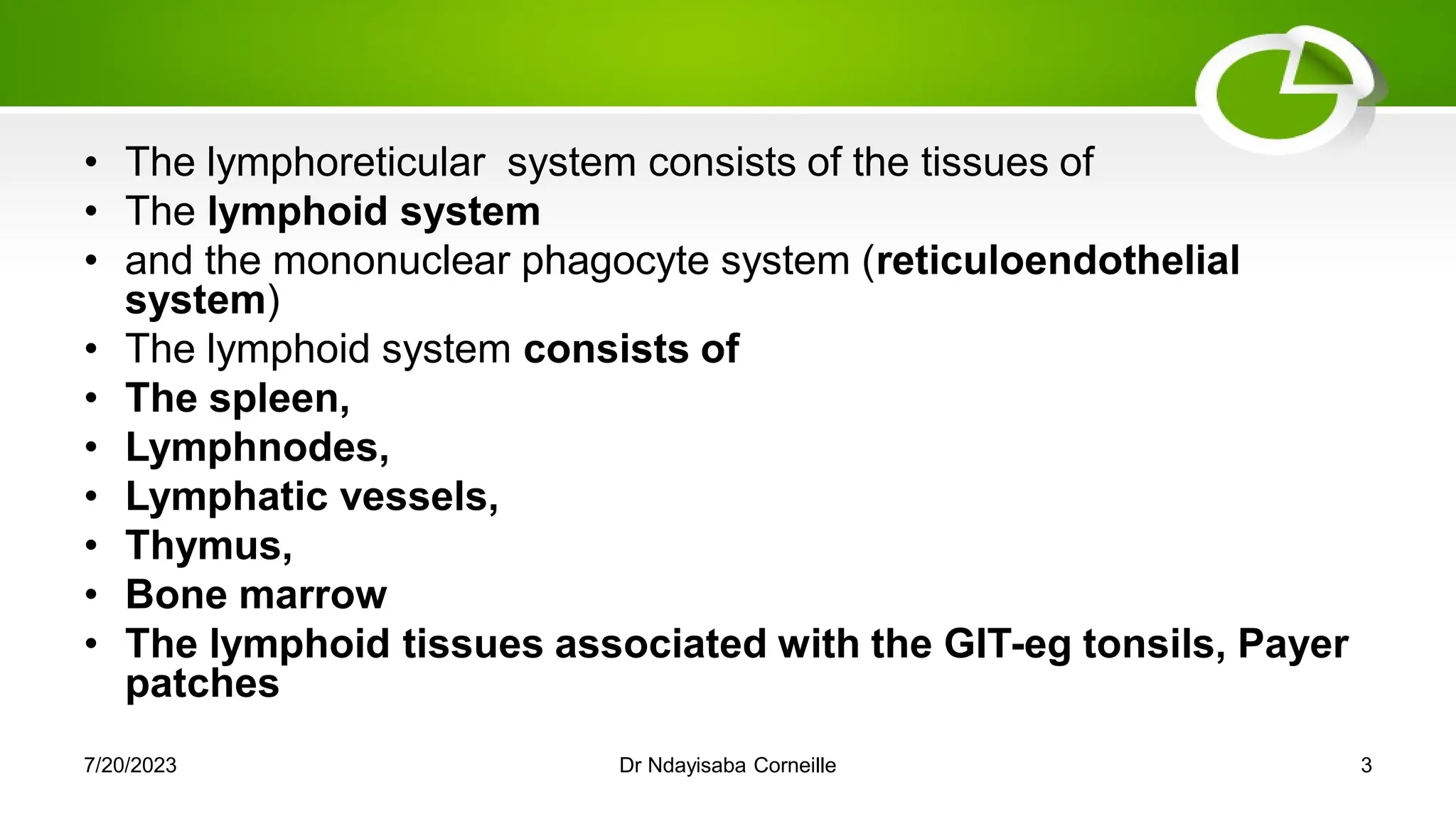
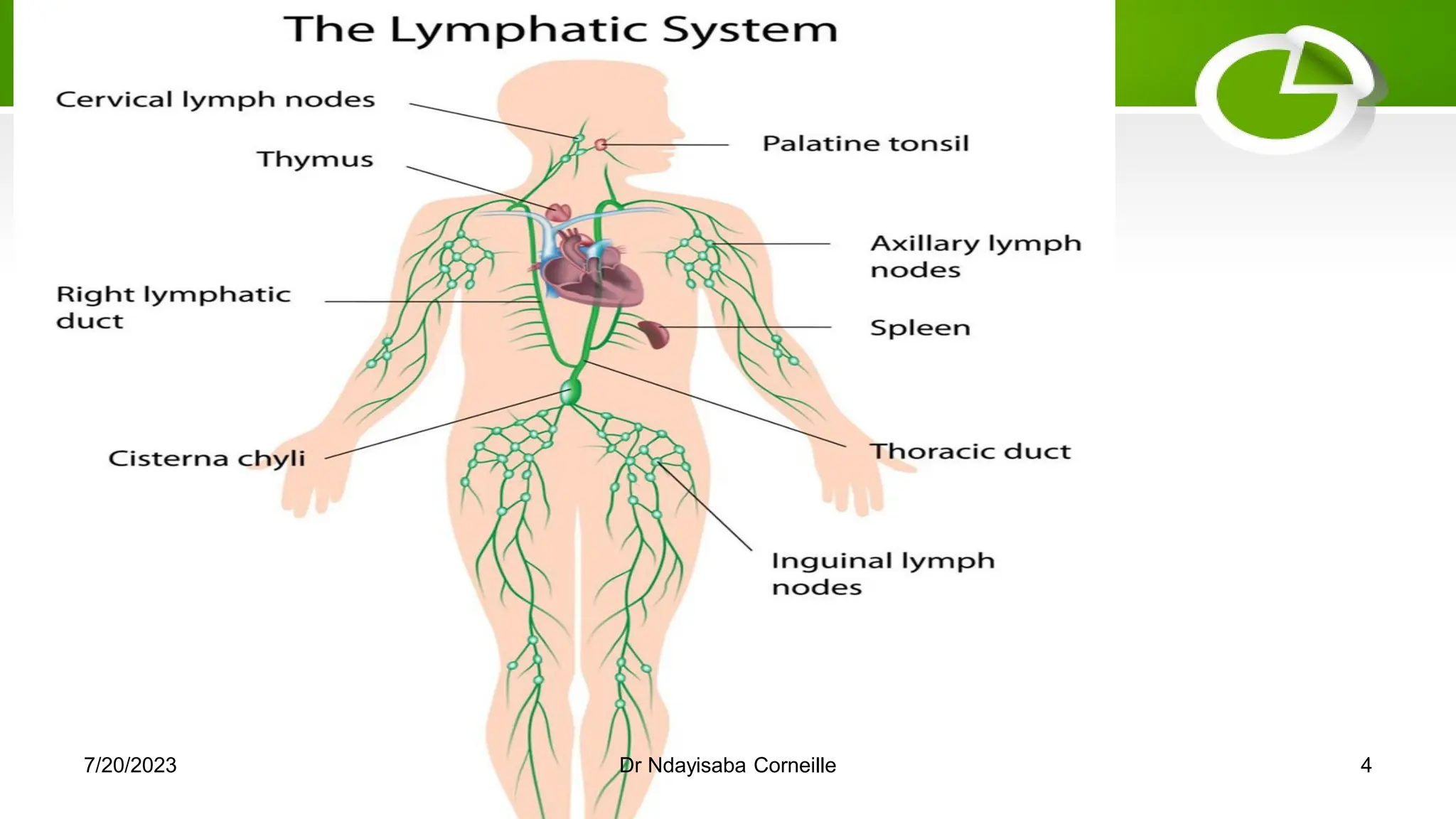
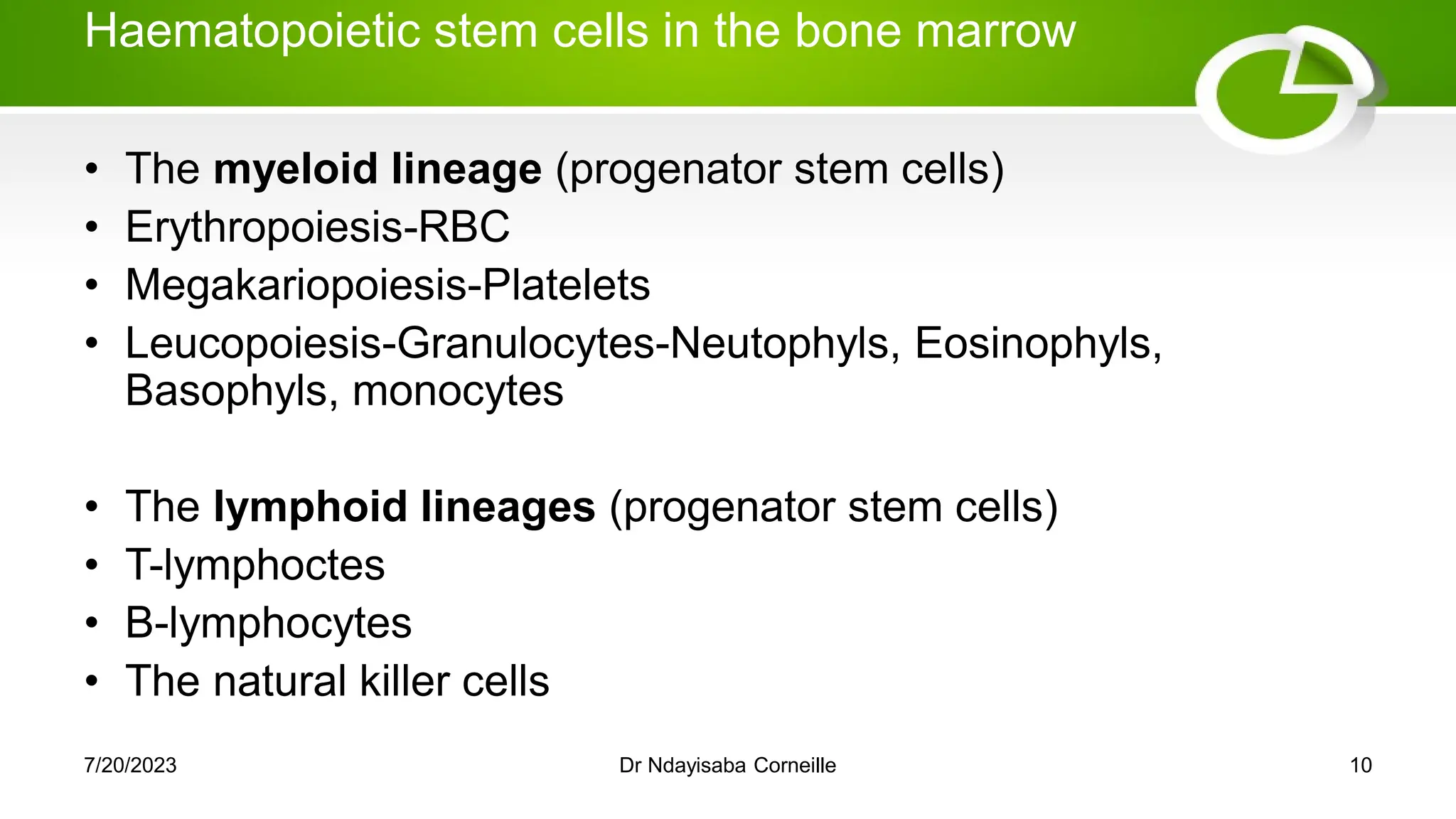
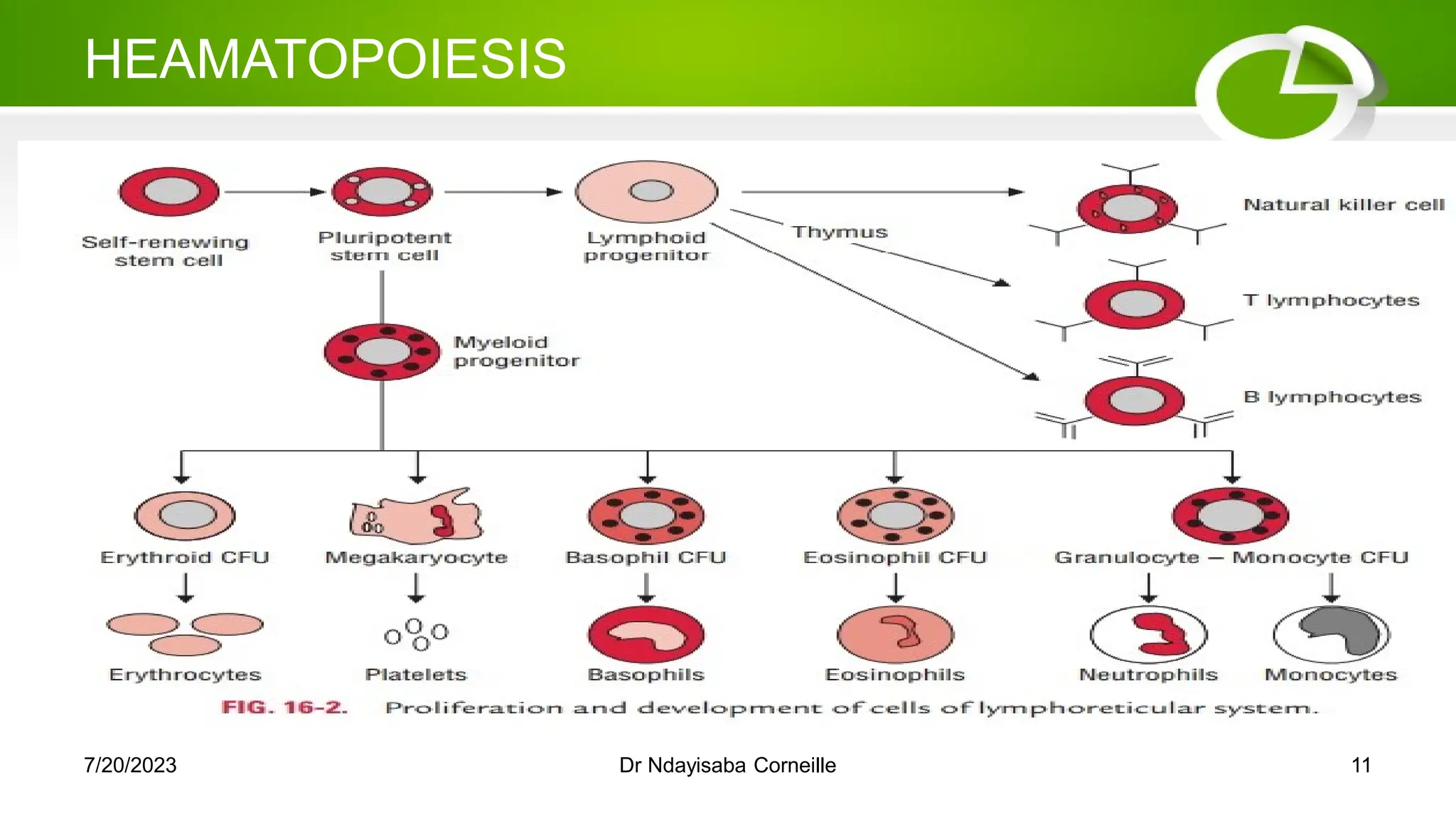
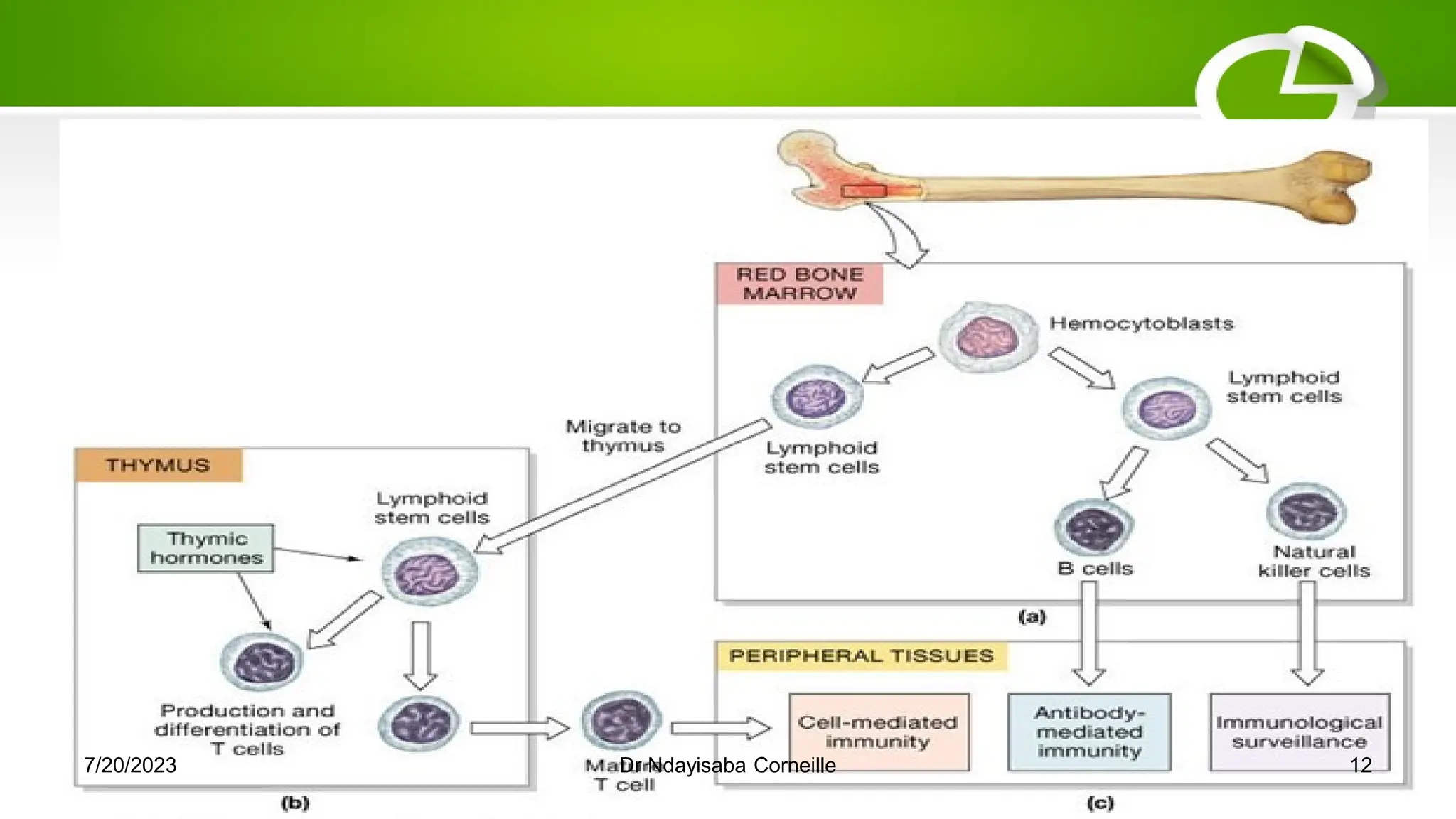
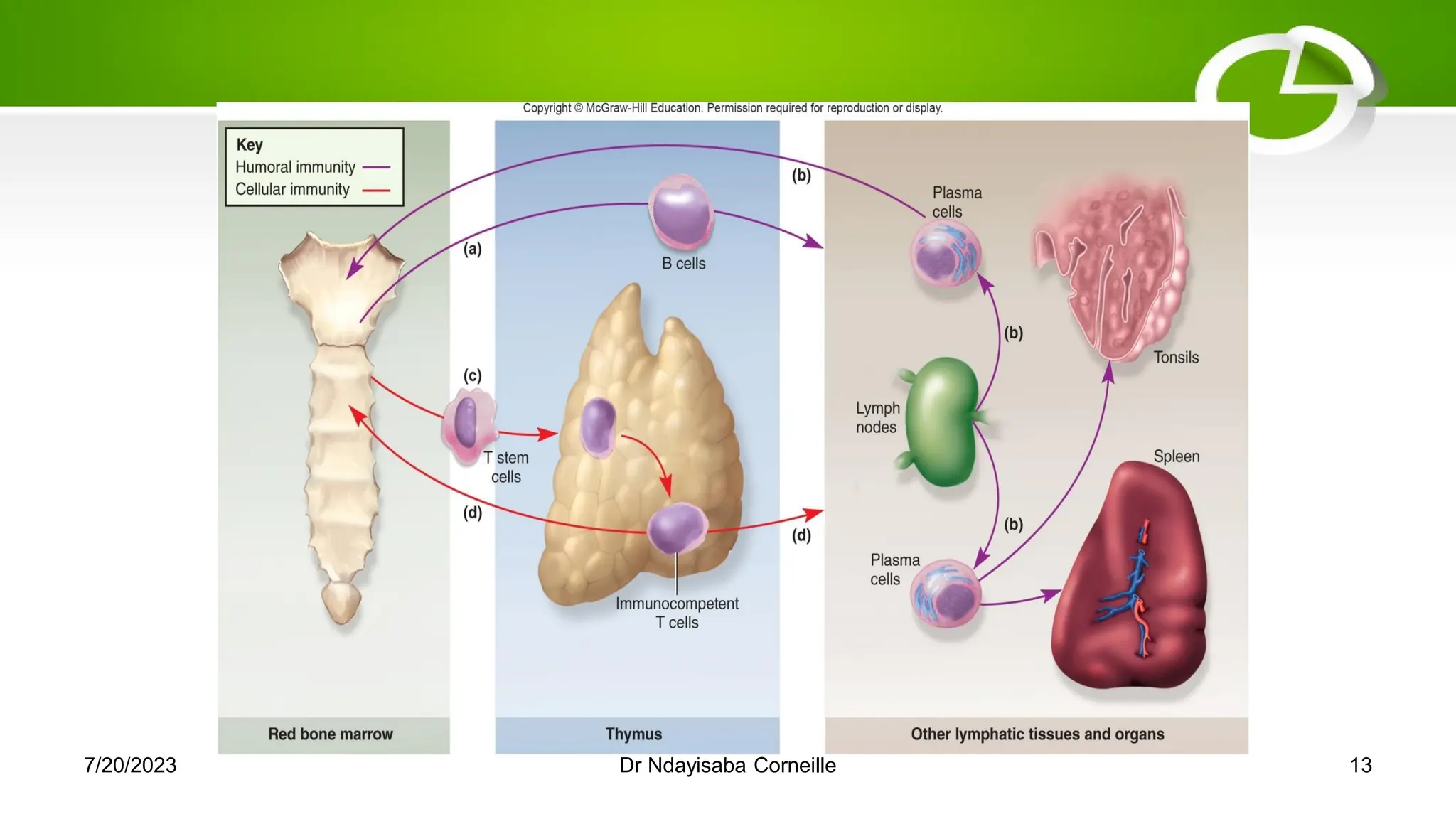
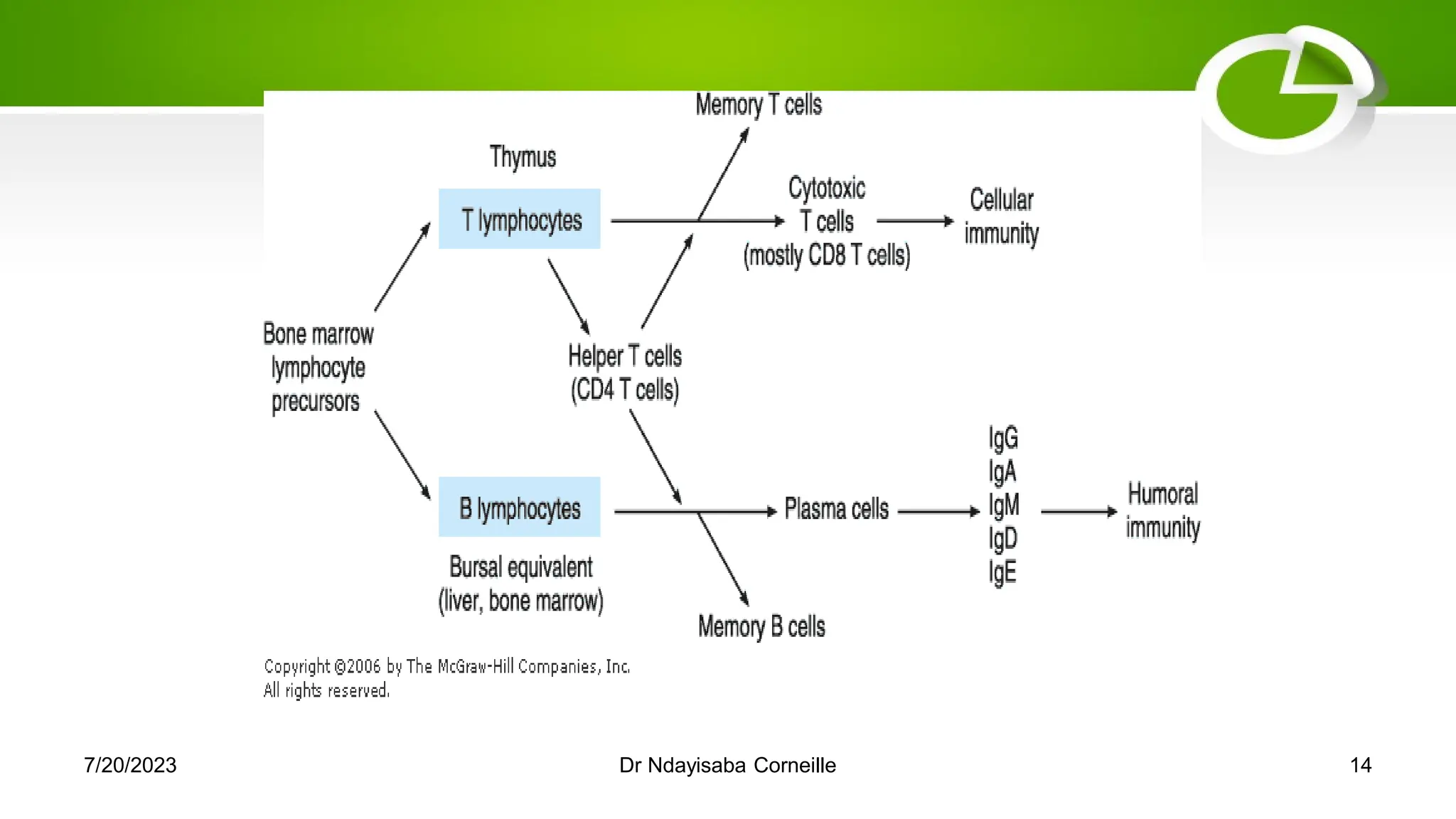
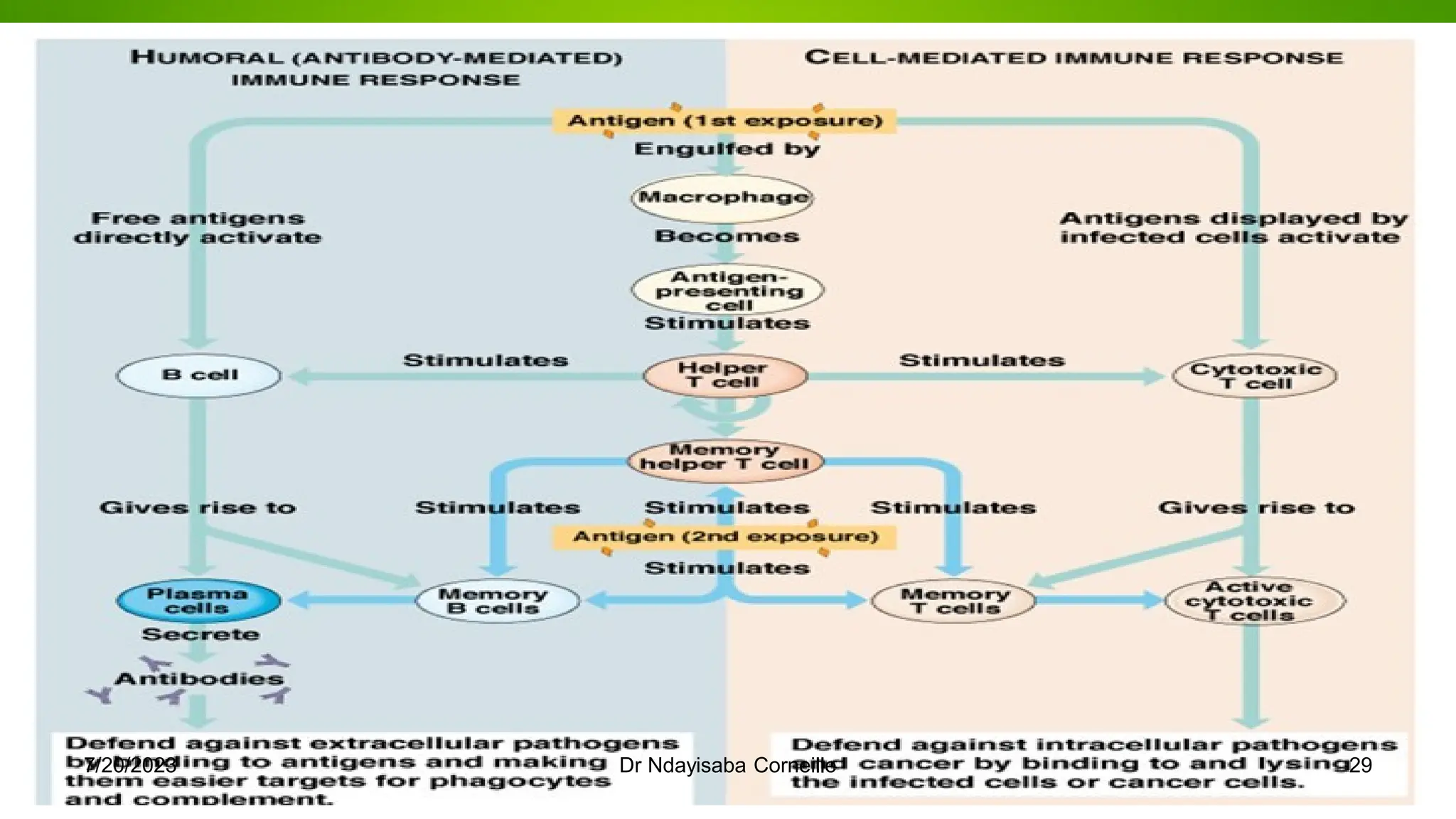
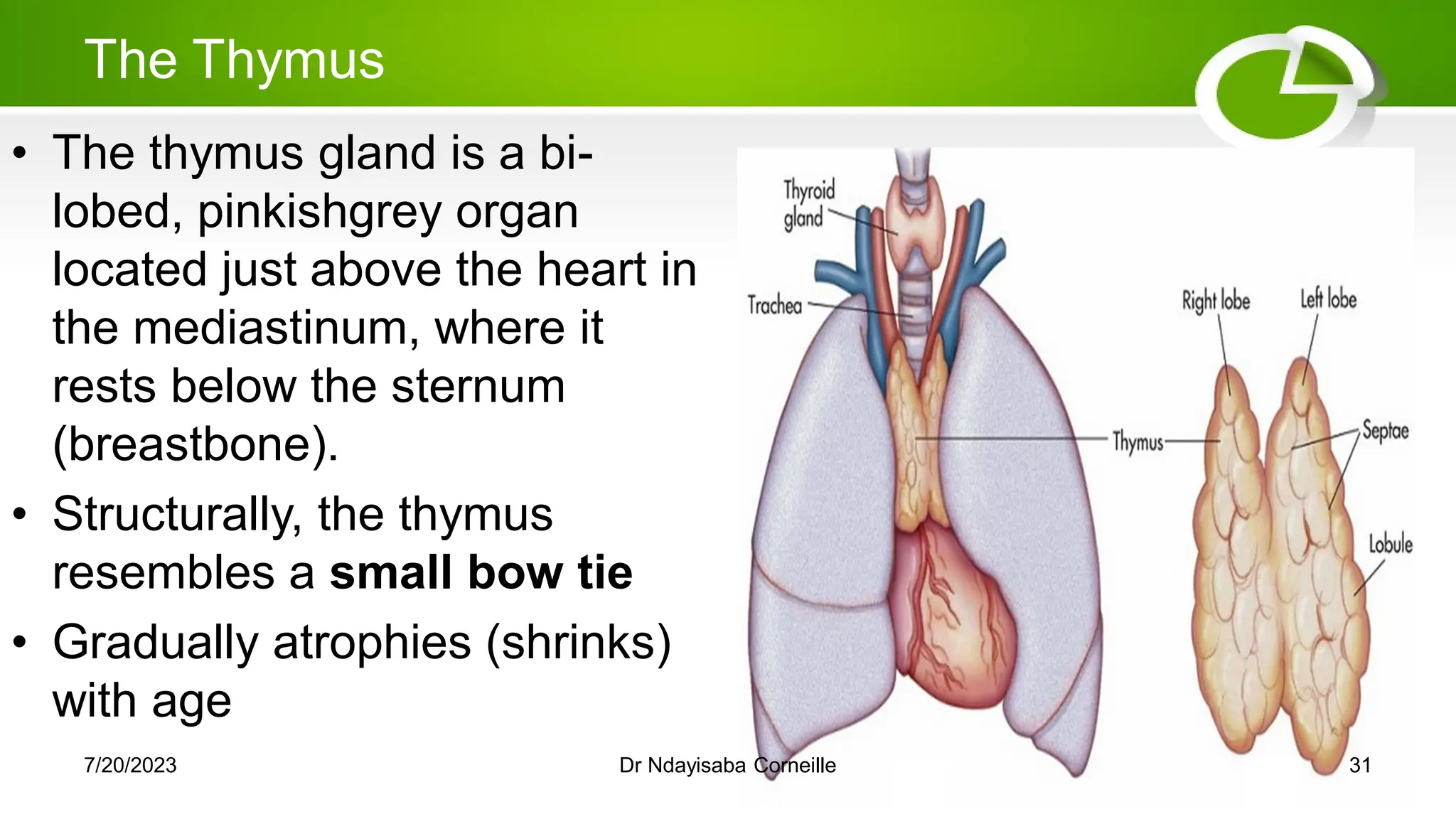
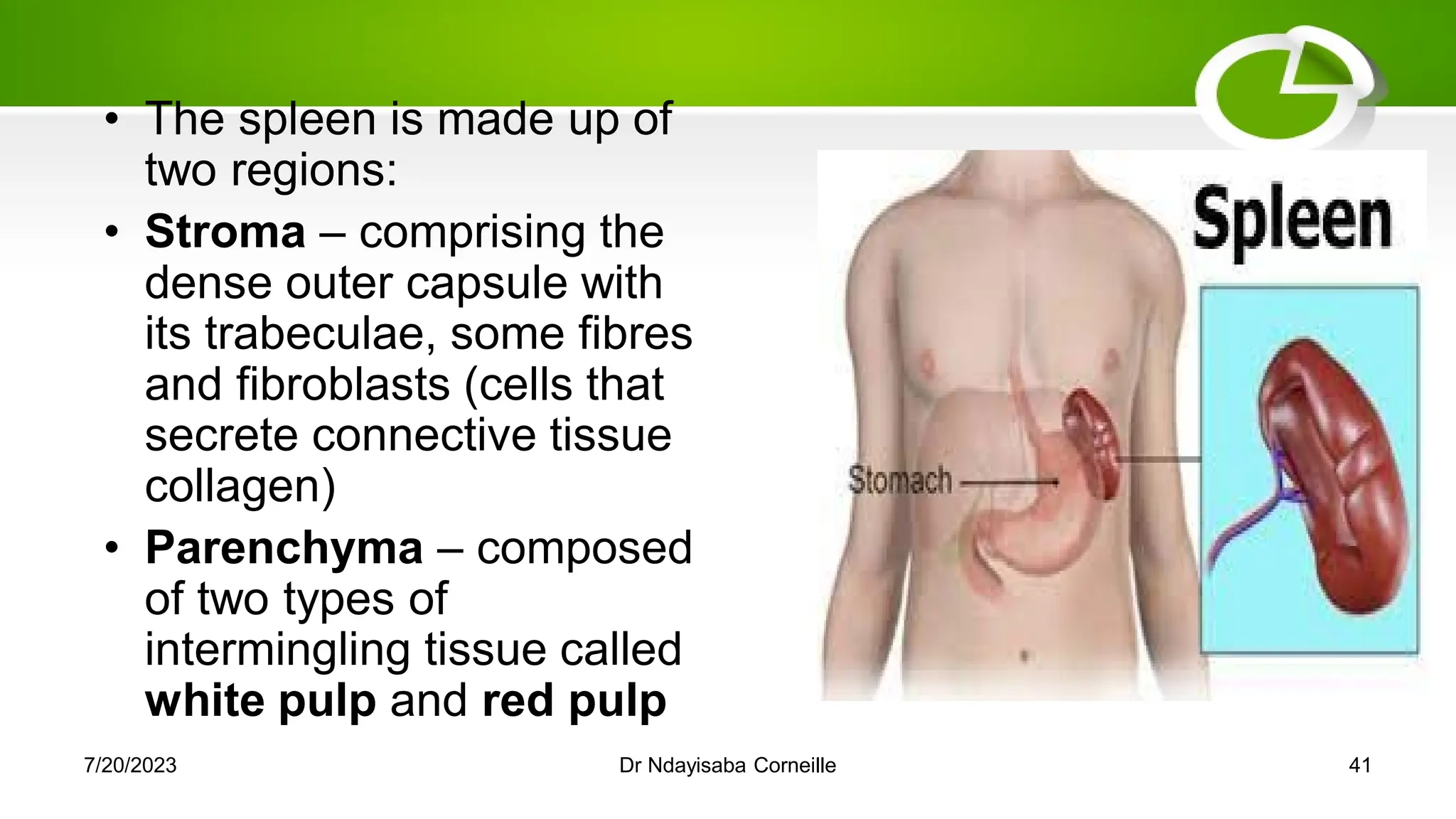
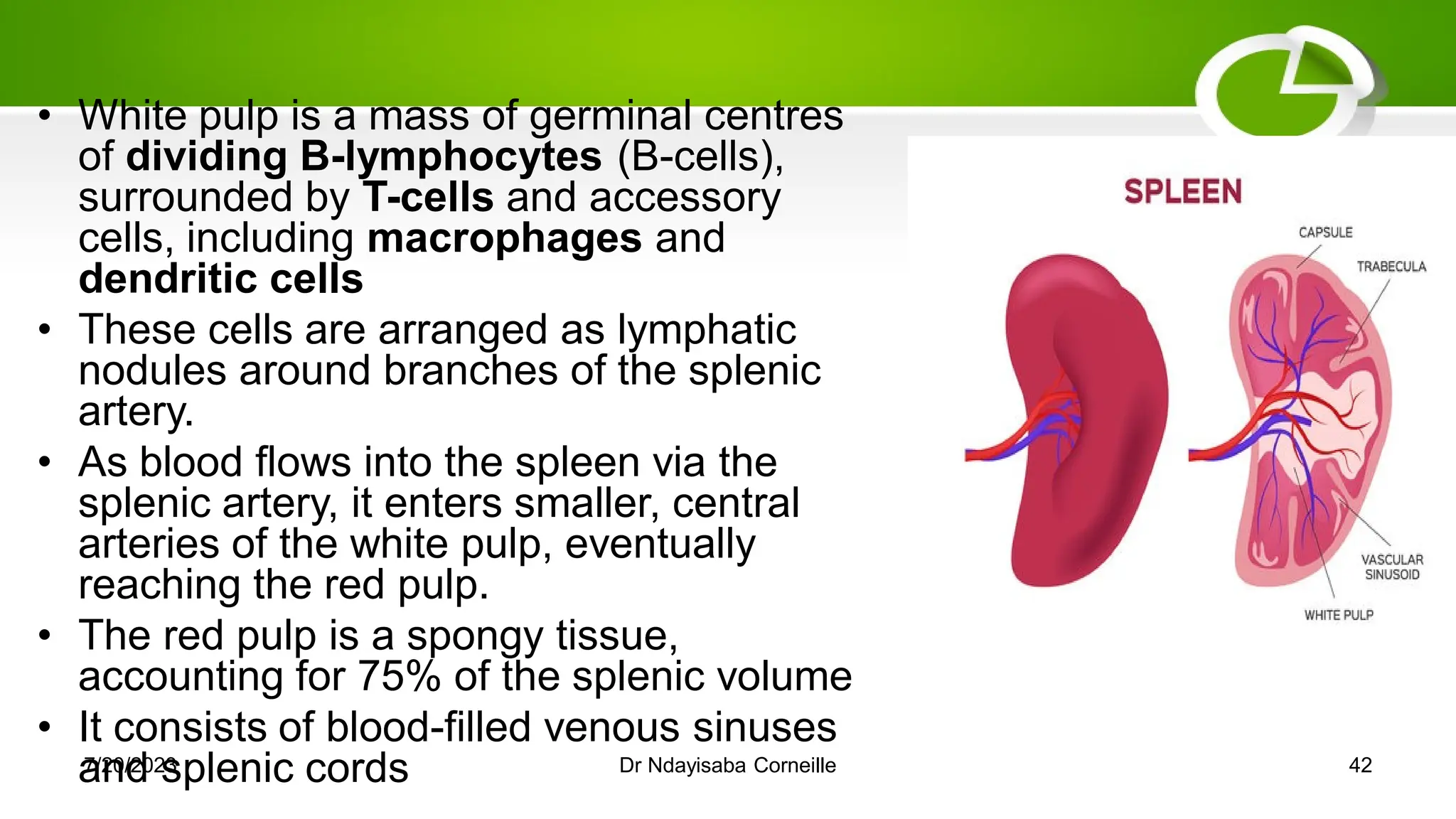
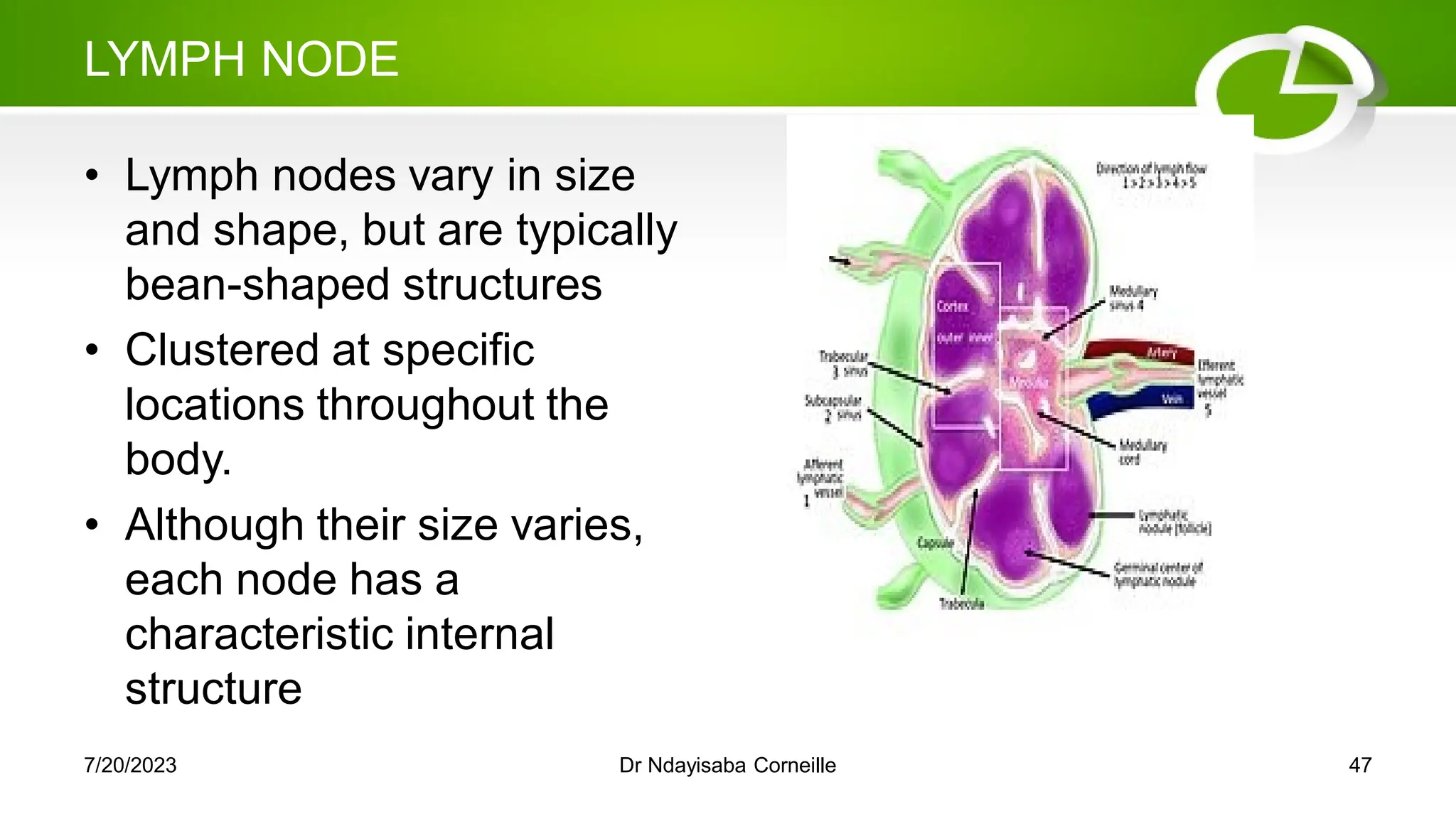
The lymphoreticular system encompasses the lymphoid and mononuclear phagocyte systems and includes primary organs like bone marrow and thymus, where T and B cells mature. Its functions include the transportation of fluids and fats, as well as immune defense through the activation of immune responses and the filtering of foreign materials. Key components are lymphocytes, antigen-presenting cells, and structures such as the spleen and lymph nodes that facilitate immune activities.