1) History taking is an essential nursing skill that provides information to make an accurate diagnosis. It involves obtaining a patient narrative through structured questioning.
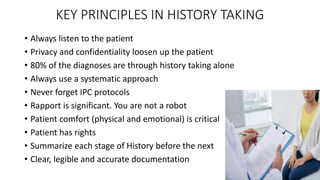
2) Key principles of history taking include actively listening to the patient, maintaining privacy and confidentiality, using a systematic approach, and ensuring patient comfort.
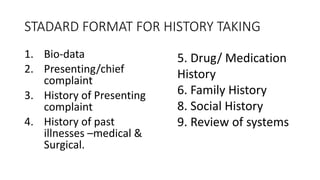
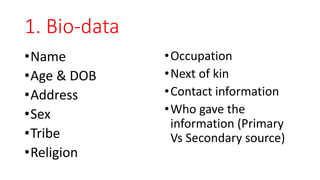
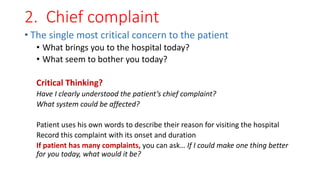
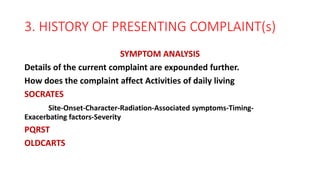
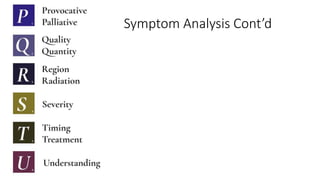
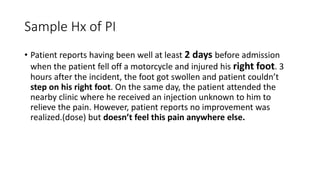
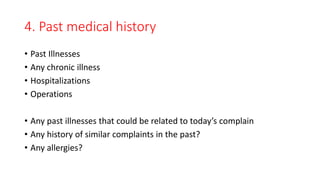
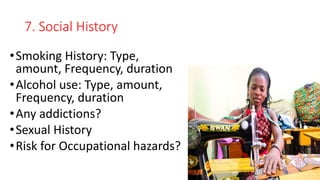
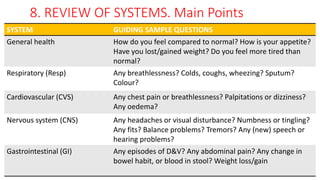
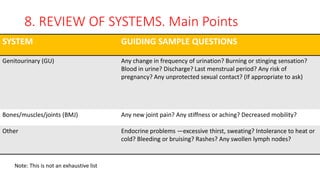
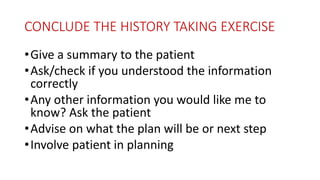
3) The standard format includes collecting biographical data, chief complaint, history of present complaint, past medical history, medication history, family history, and reviewing all body systems. Summarizing each section ensures clear understanding before moving forward.