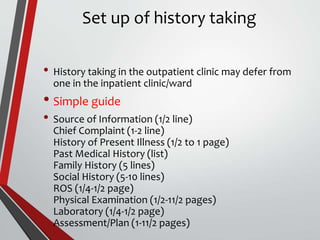
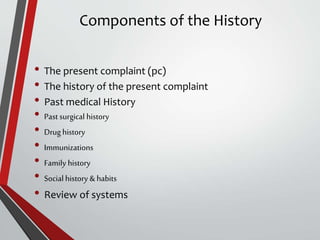
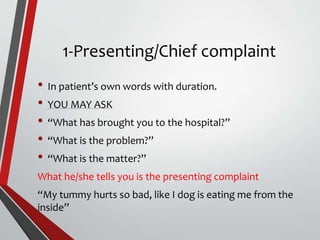
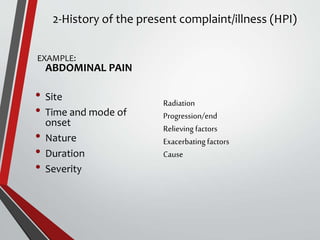
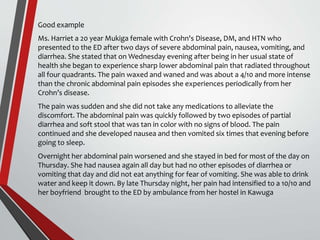
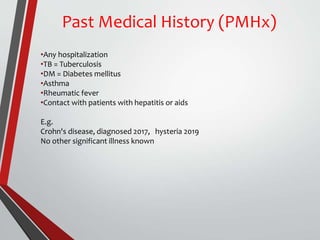
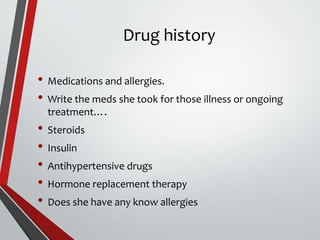
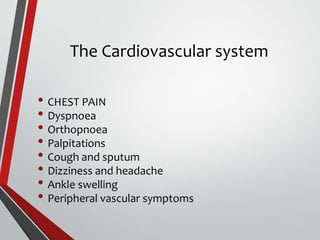
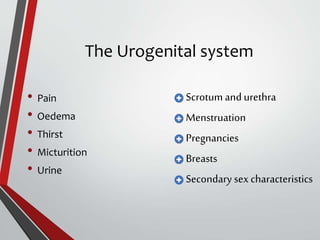
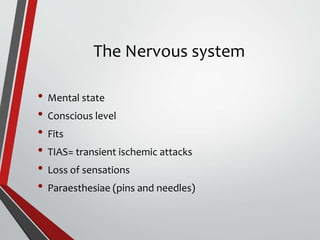
The document outlines the process and importance of health history taking, emphasizing a holistic assessment of factors affecting a patient's health, including social and familial influences. It provides a structured guide for healthcare professionals to document pertinent information, including presenting complaints, medical history, and review of systems. The ultimate goal of thorough history taking is to aid in accurate diagnosis and effective patient management.