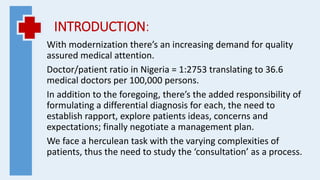
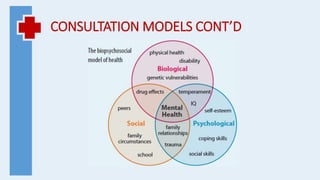
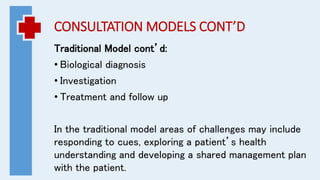
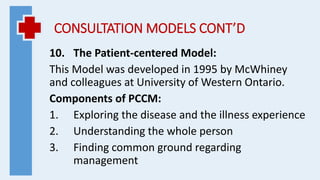
The document provides an overview of consultation models and communication skills used in medical consultations. It defines consultation as an interactive session where a healthy or sick individual seeks explanation, cure, or advice from a physician. The document outlines 10 consultation models that guide the structure and components of a consultation, including the patient-centered model. It emphasizes using communication skills and considering biopsychosocial factors to conduct effective consultations that improve patient satisfaction and adherence.