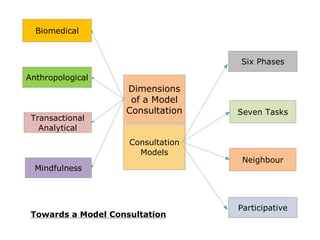
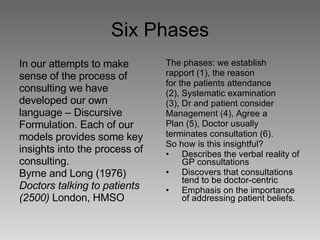
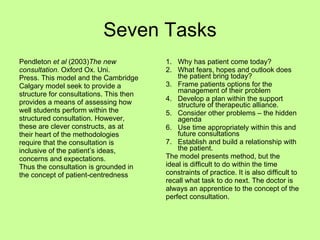
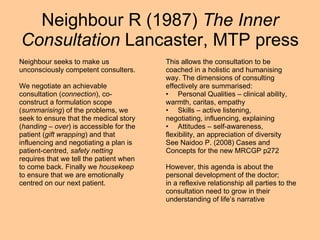
The document explores the complexities of biomedical consultations, emphasizing the need for clinicians to address patients' fears and expectations alongside their medical reasoning. It discusses various models of consultation and the importance of patient-centeredness, emotional intelligence, and the therapeutic alliance in achieving effective communication. Additionally, it suggests that narrative-based medicine can aid in reframing patients' stories to foster deeper understanding and co-creation of care plans.