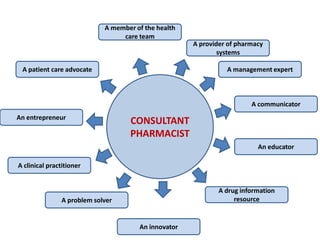
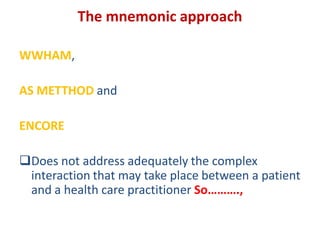
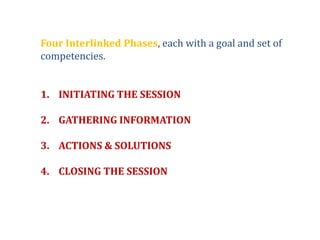
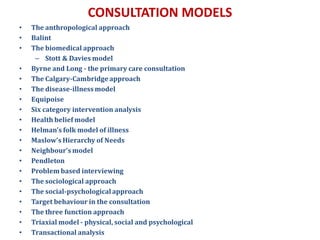
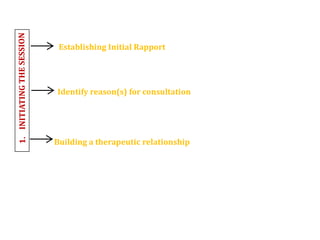
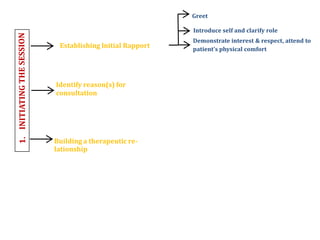
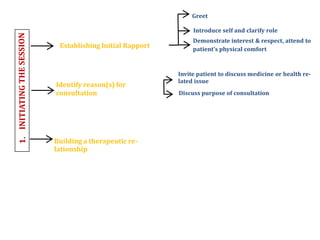
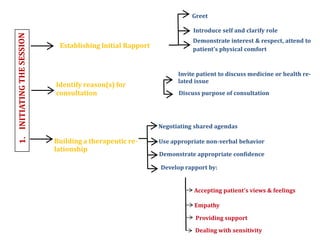
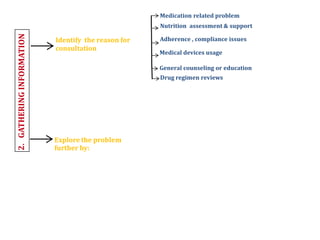
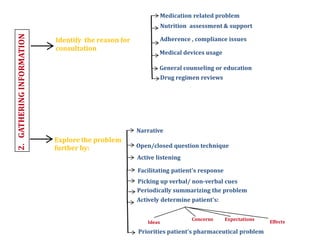
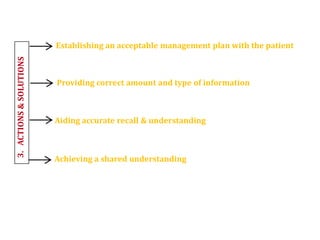
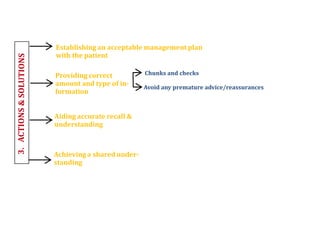
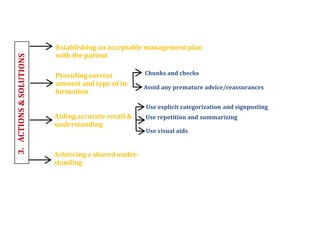
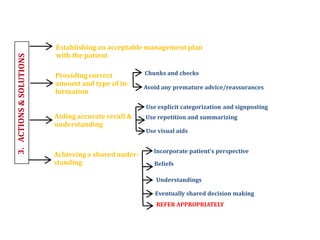
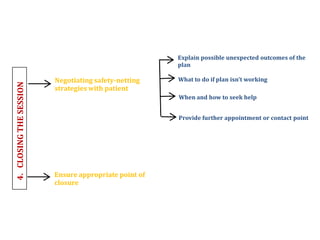
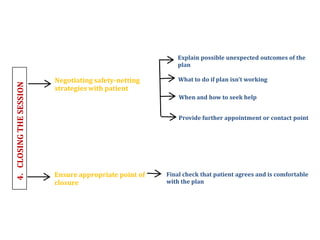
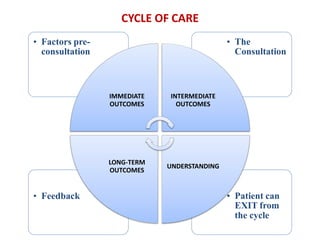
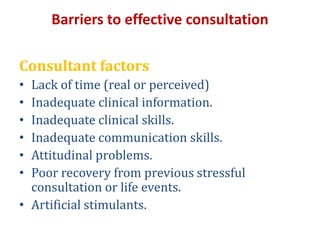
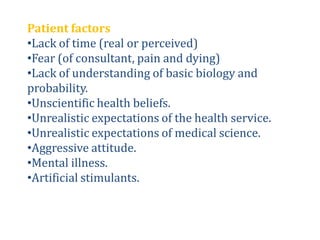
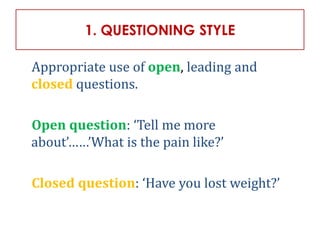
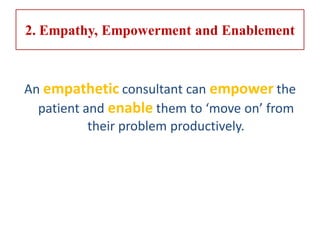
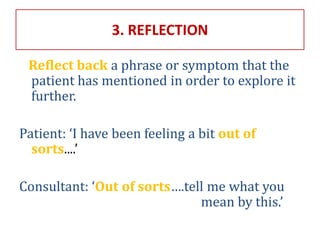
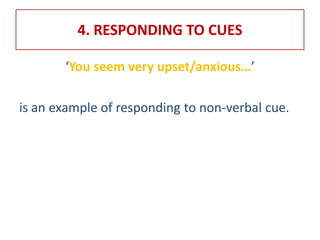
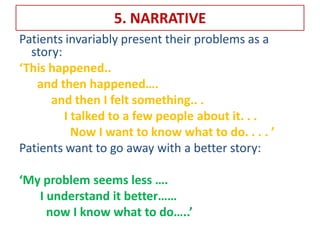
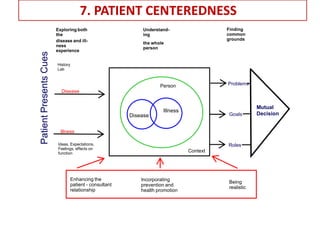
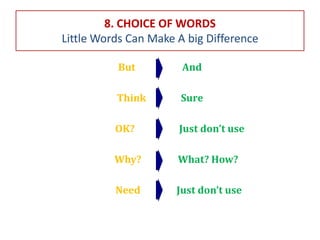
The document discusses the role and importance of consultant pharmacists in diabetes management, emphasizing effective communication and the patient consultancy process. It outlines various consultation models and phases, highlighting the need for establishing rapport, gathering information, and creating management plans with patients. Barriers to effective consultation and the skills required for successful interaction are also addressed.