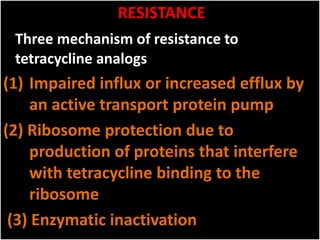
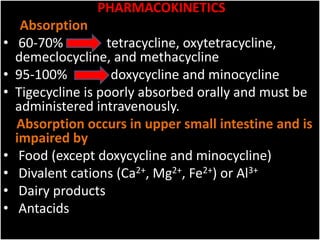
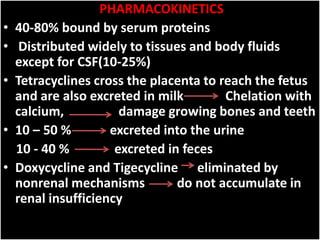
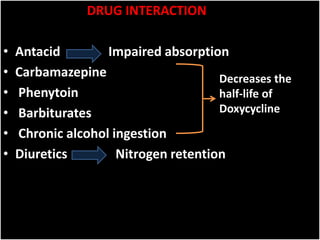
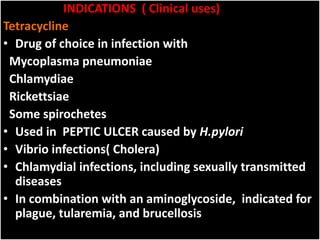
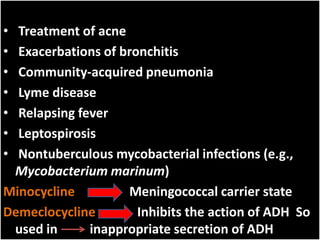
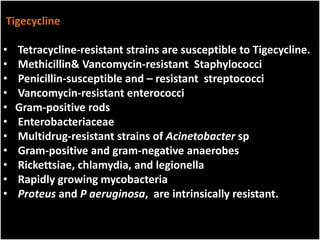
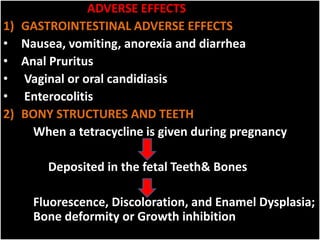
Tetracyclines are a class of broad-spectrum bacteriostatic antibiotics that work by binding to the 30S subunit of bacterial ribosomes and inhibiting protein synthesis. They are effective against many gram-positive and gram-negative bacteria, as well as anaerobes, rickettsiae, chlamydiae, mycoplasmas, and protozoa. Tetracyclines have a range of pharmacokinetic properties from short-acting to long-acting drugs. They are subject to resistance via efflux pumps, ribosomal protection proteins, and enzymatic inactivation. Common adverse effects include gastrointestinal issues, staining of teeth and bones, and photosensitivity.