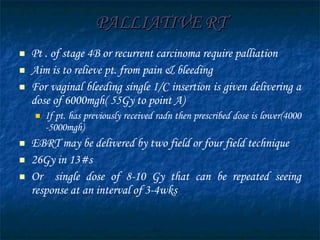
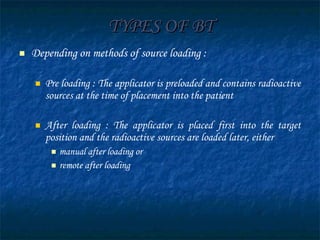
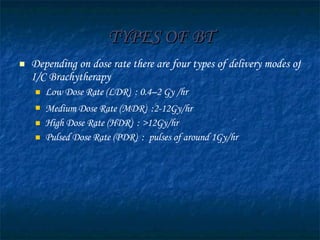
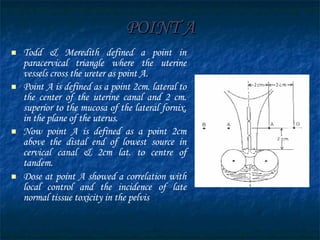
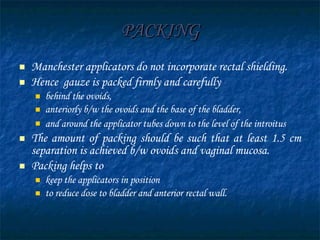
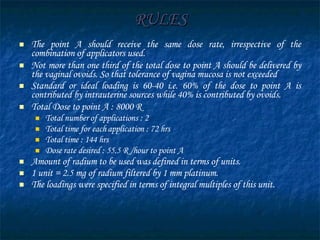
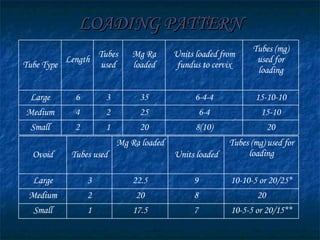
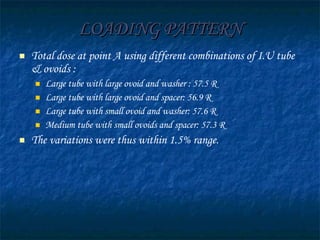
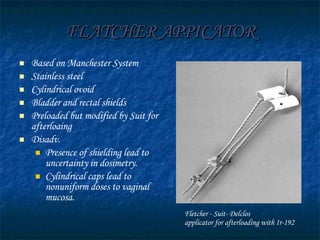
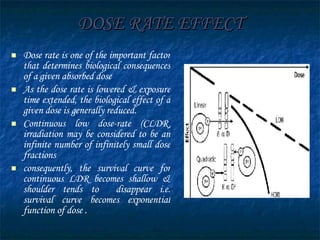
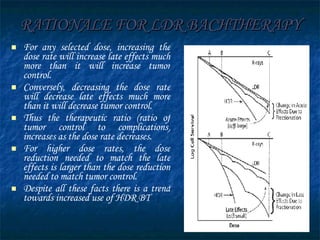
This document discusses teletherapy and brachytherapy for the treatment of cervical cancer. It provides details on the Manchester brachytherapy system, which standardized dose specification by defining the dose delivered to a single point (Point A) located 2cm lateral to the cervical os and 2cm along the uterine canal. This allowed for reproducible and comparable dose delivery across patients regardless of applicator size or positioning. The document also outlines other historical brachytherapy systems and the advantages of intracavitary brachytherapy for cervical cancer treatment.