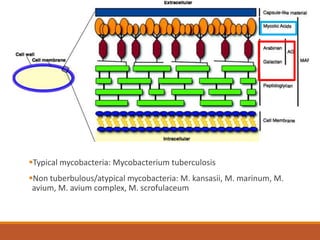
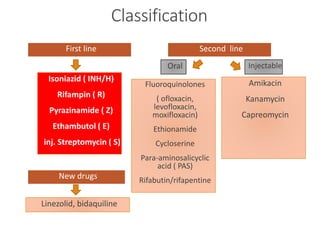
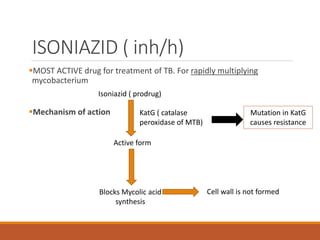
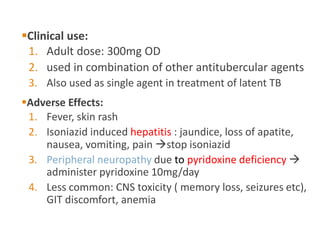
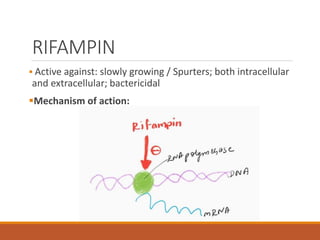
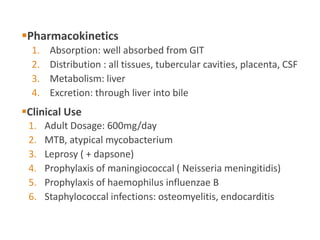
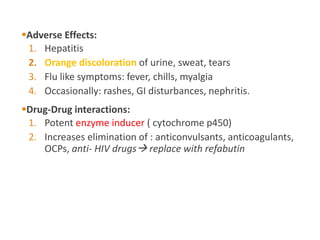
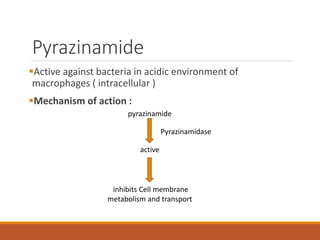
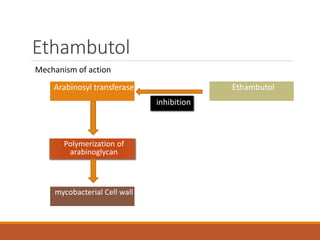
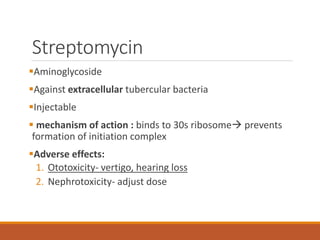
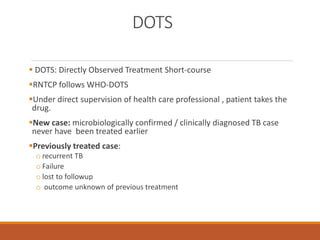
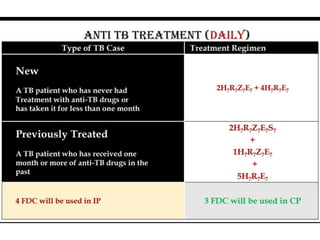
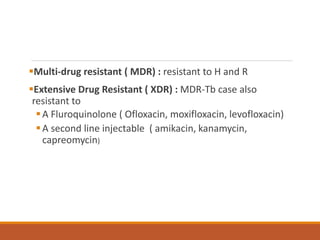
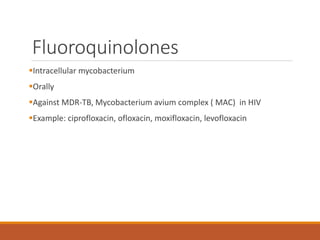
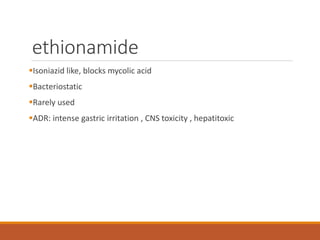
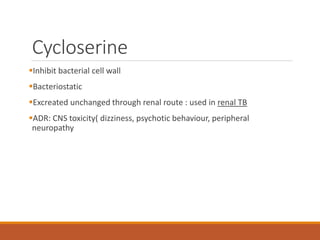
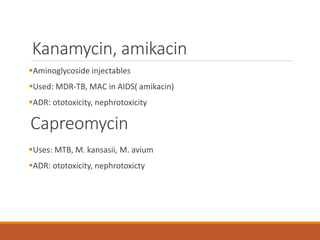
This document summarizes anti-tuberculosis therapy (ATT). It describes the typical and atypical mycobacteria treated by ATT. The first and second line drugs used are outlined, including their mechanisms of action, pharmacokinetics, clinical uses, and adverse effects. DOTS (Directly Observed Treatment Short-course) is also summarized, which follows the WHO recommended approach of direct observation to ensure patient adherence to the drug regimen. Drug-resistant forms of tuberculosis including MDR-TB and XDR-TB are defined.