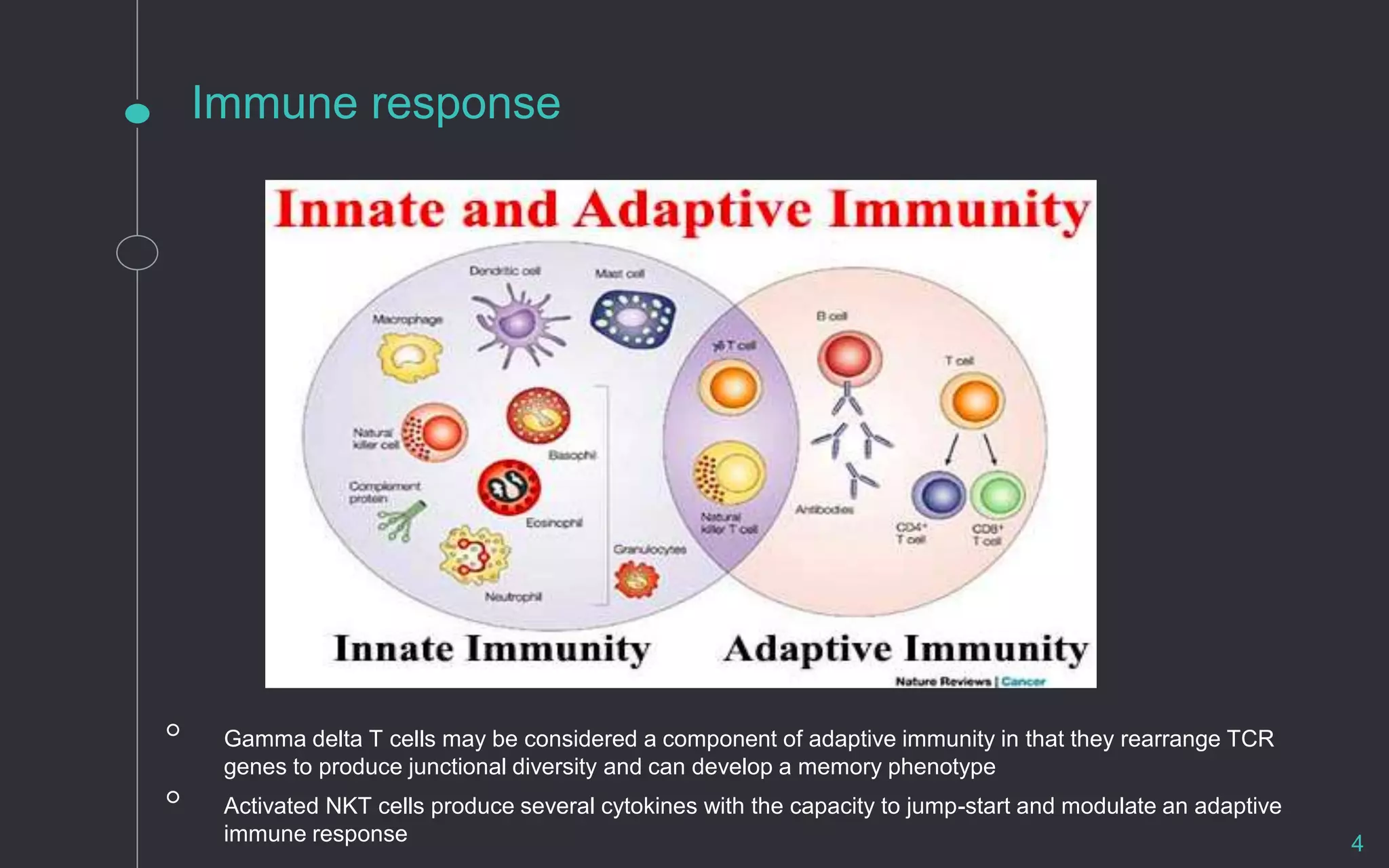
The document covers T-cell mediated immune responses, focusing on their development, selection processes, activation, and differentiation. It highlights the importance of adaptive immunity in clearing infections and includes details about T-cell precursors, thymic selection, and the role of various signaling molecules. Furthermore, the document discusses T-cell anergy, regulation, and factors influencing T-cell activation and exhaustion in chronic conditions.