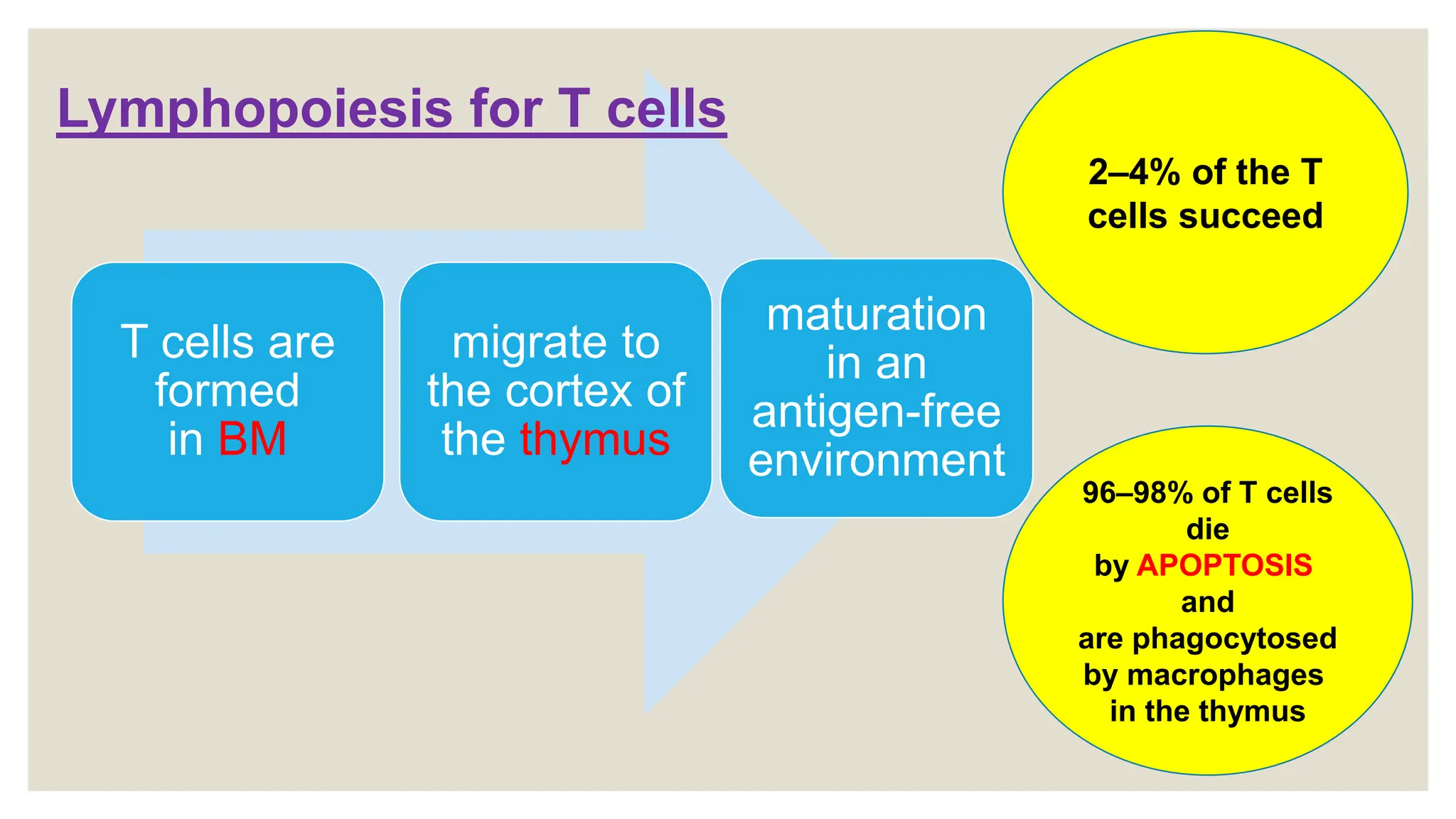
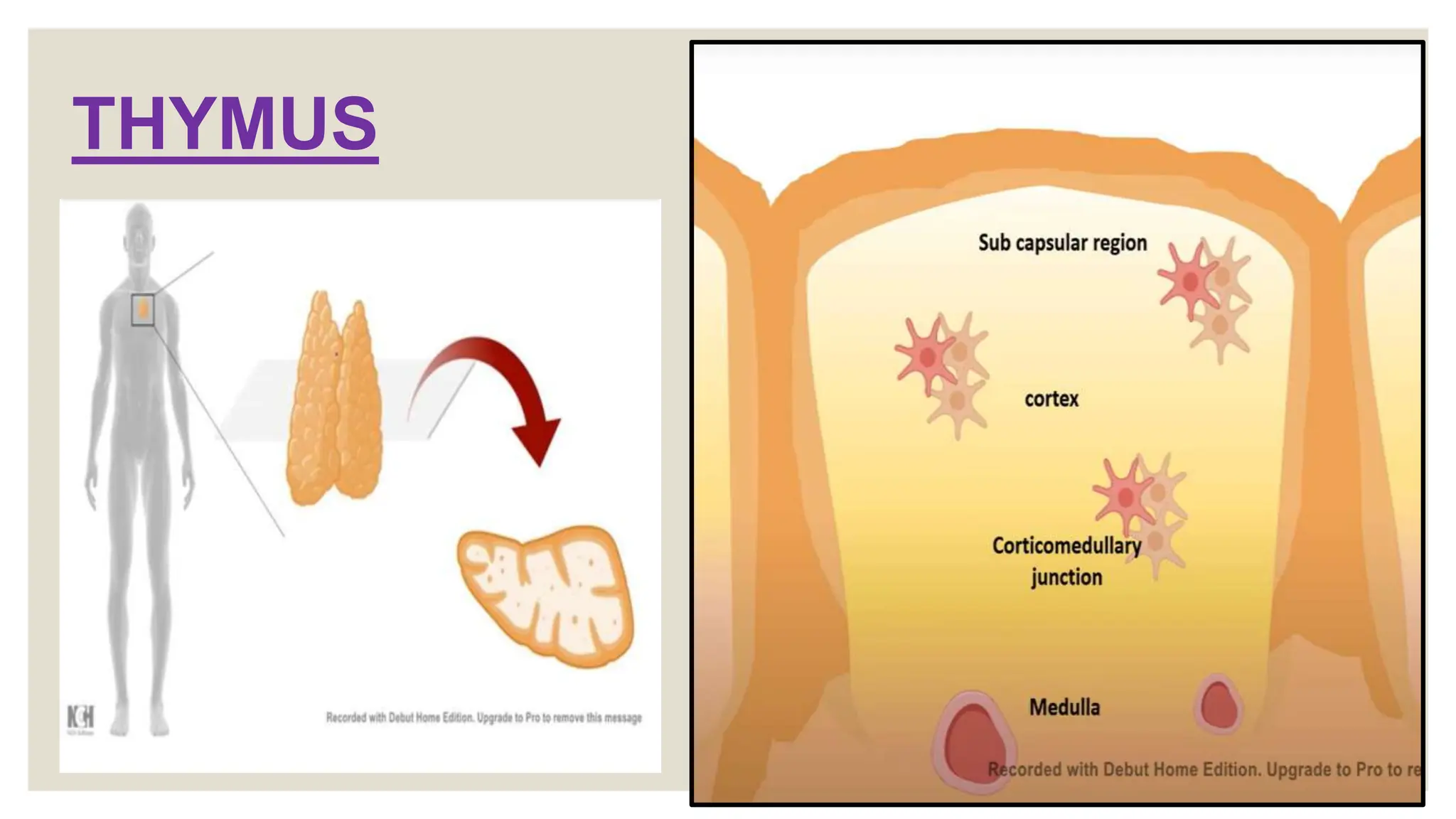
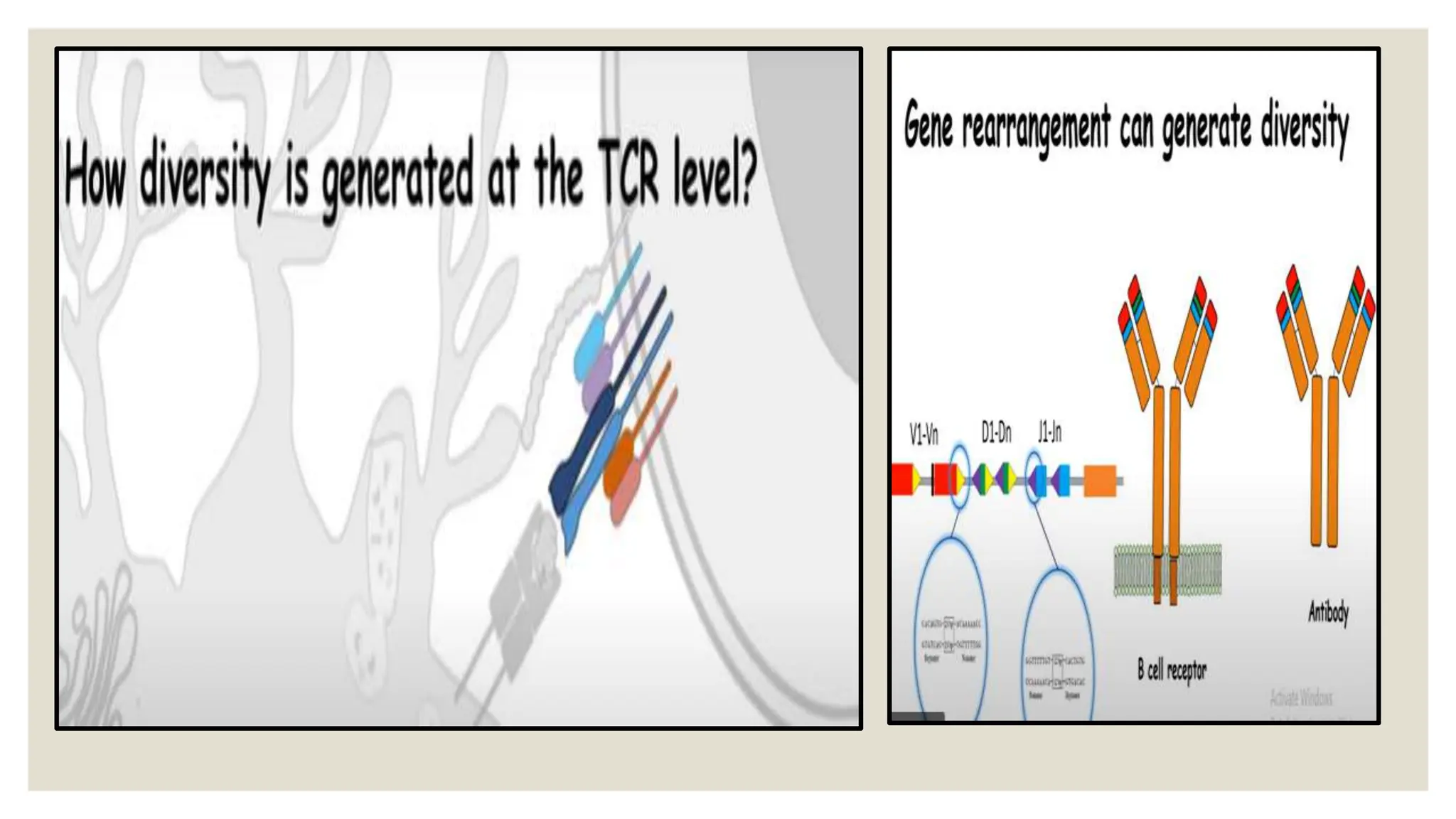
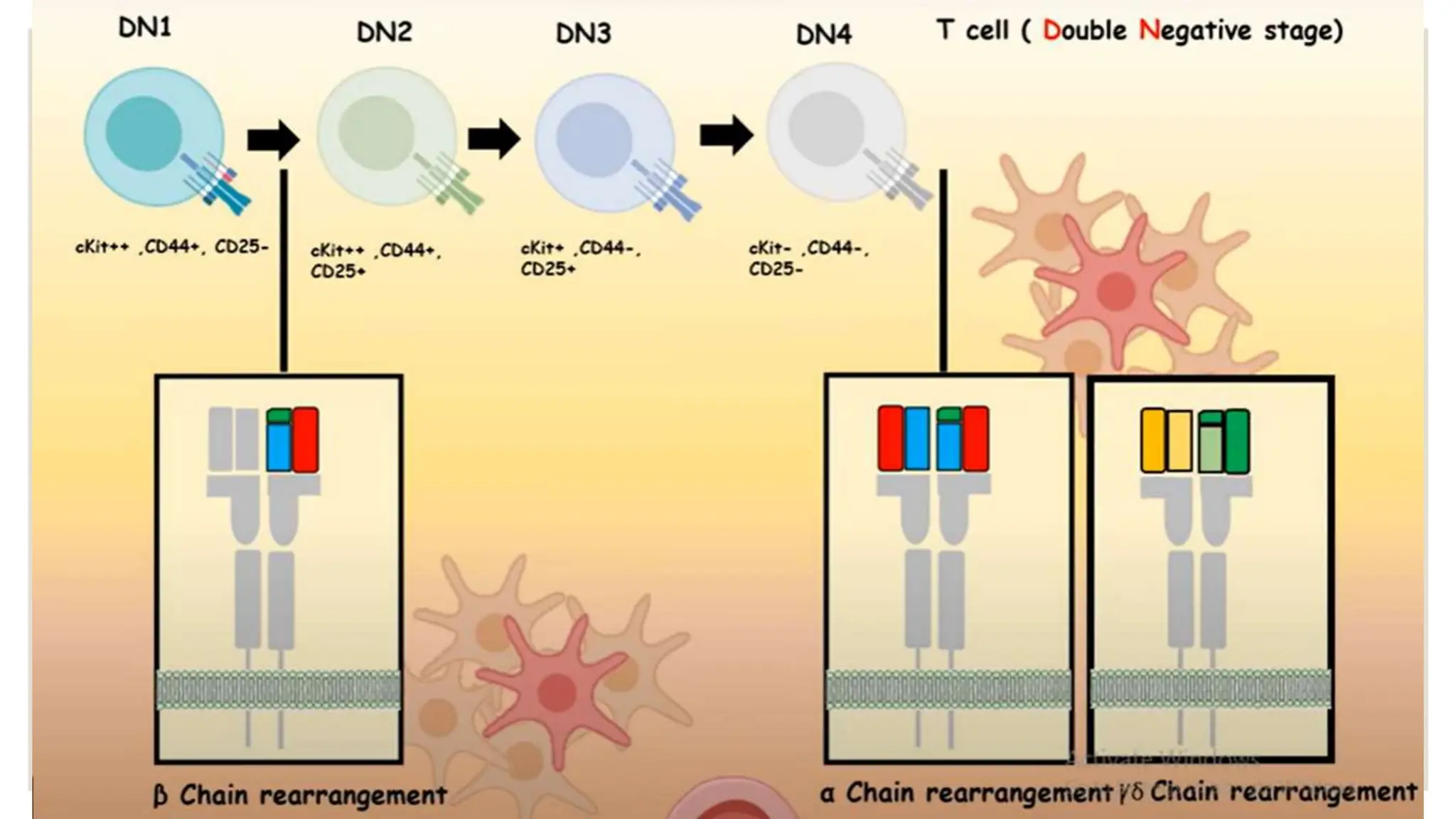
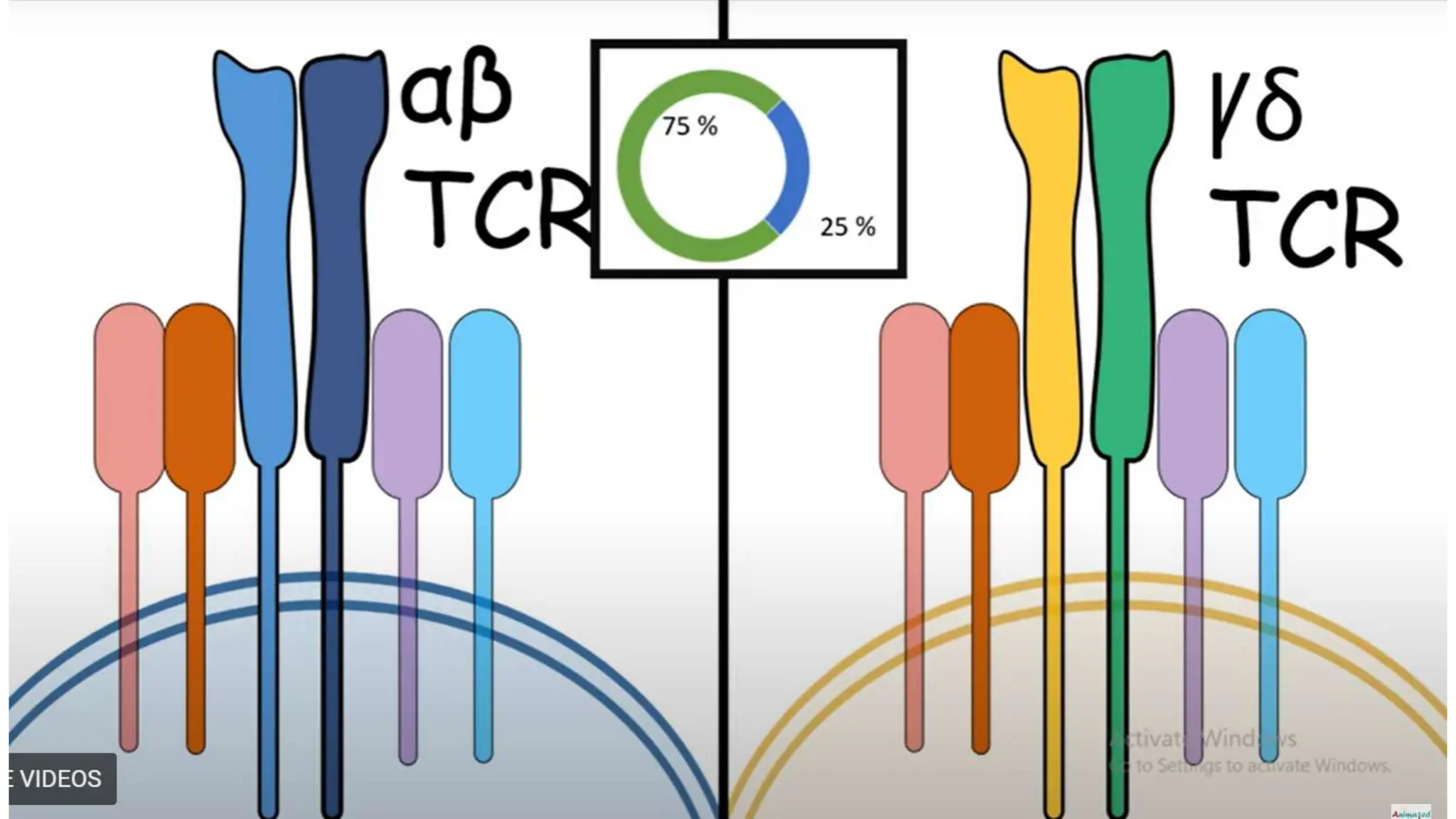
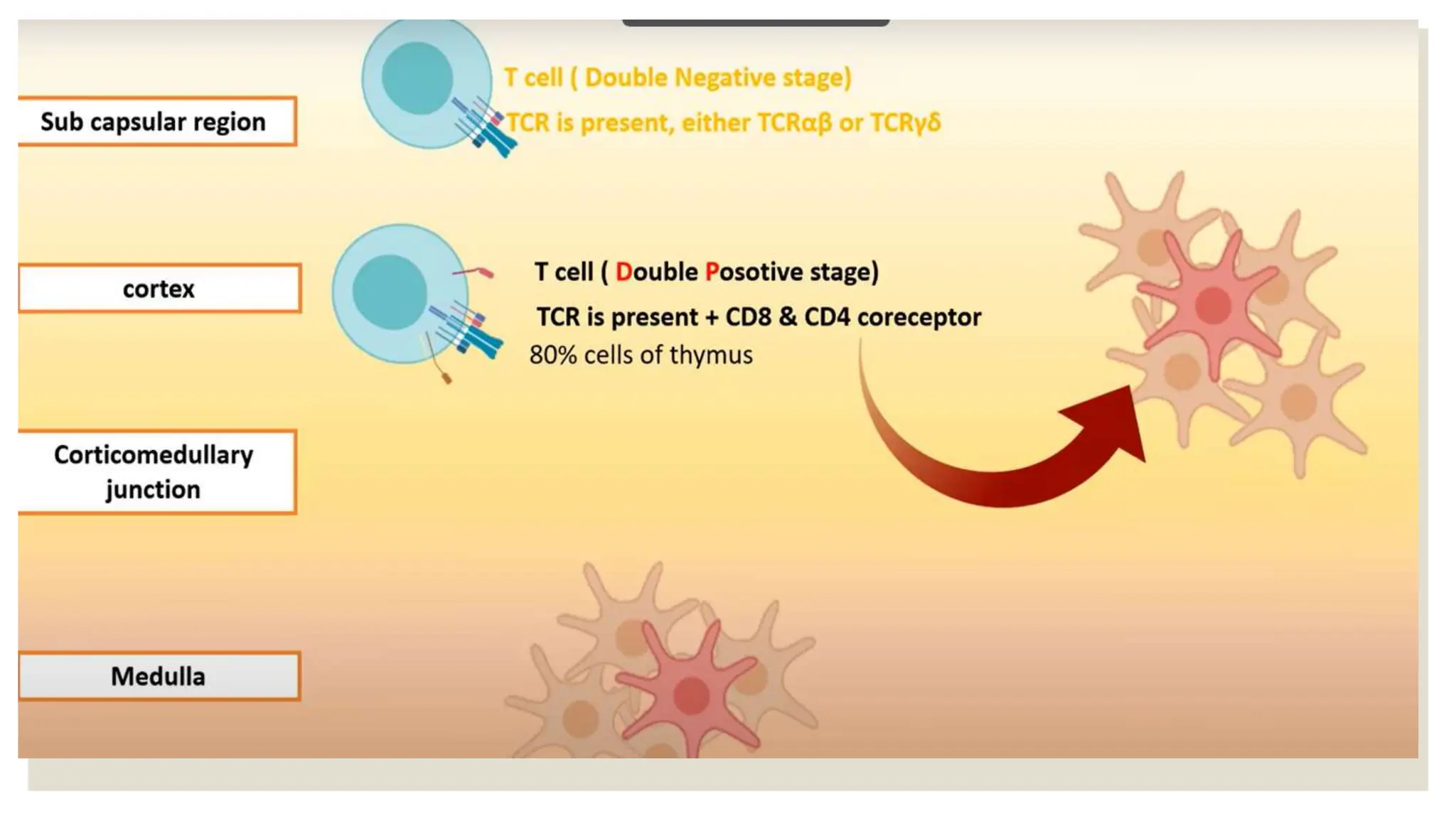
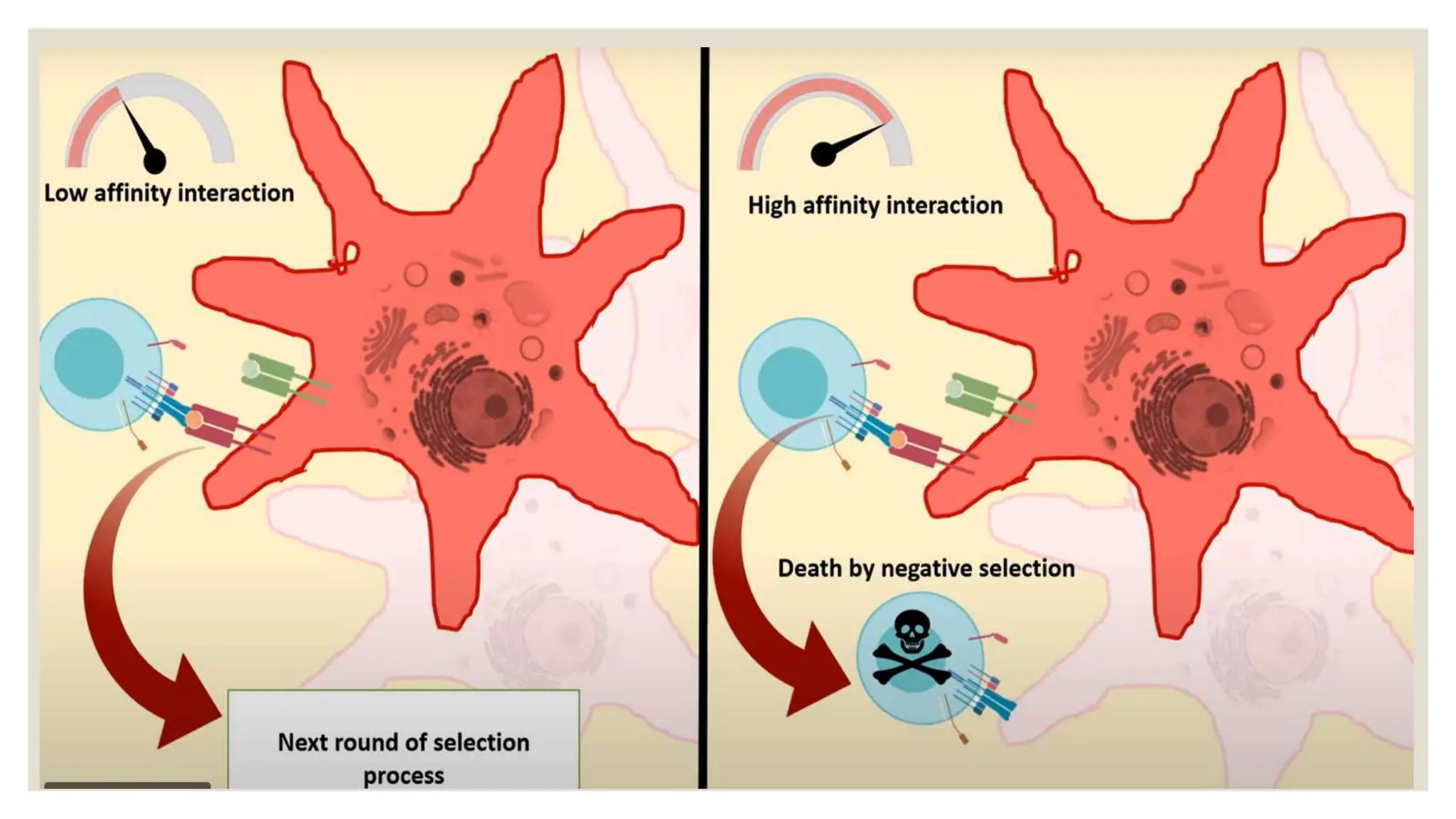
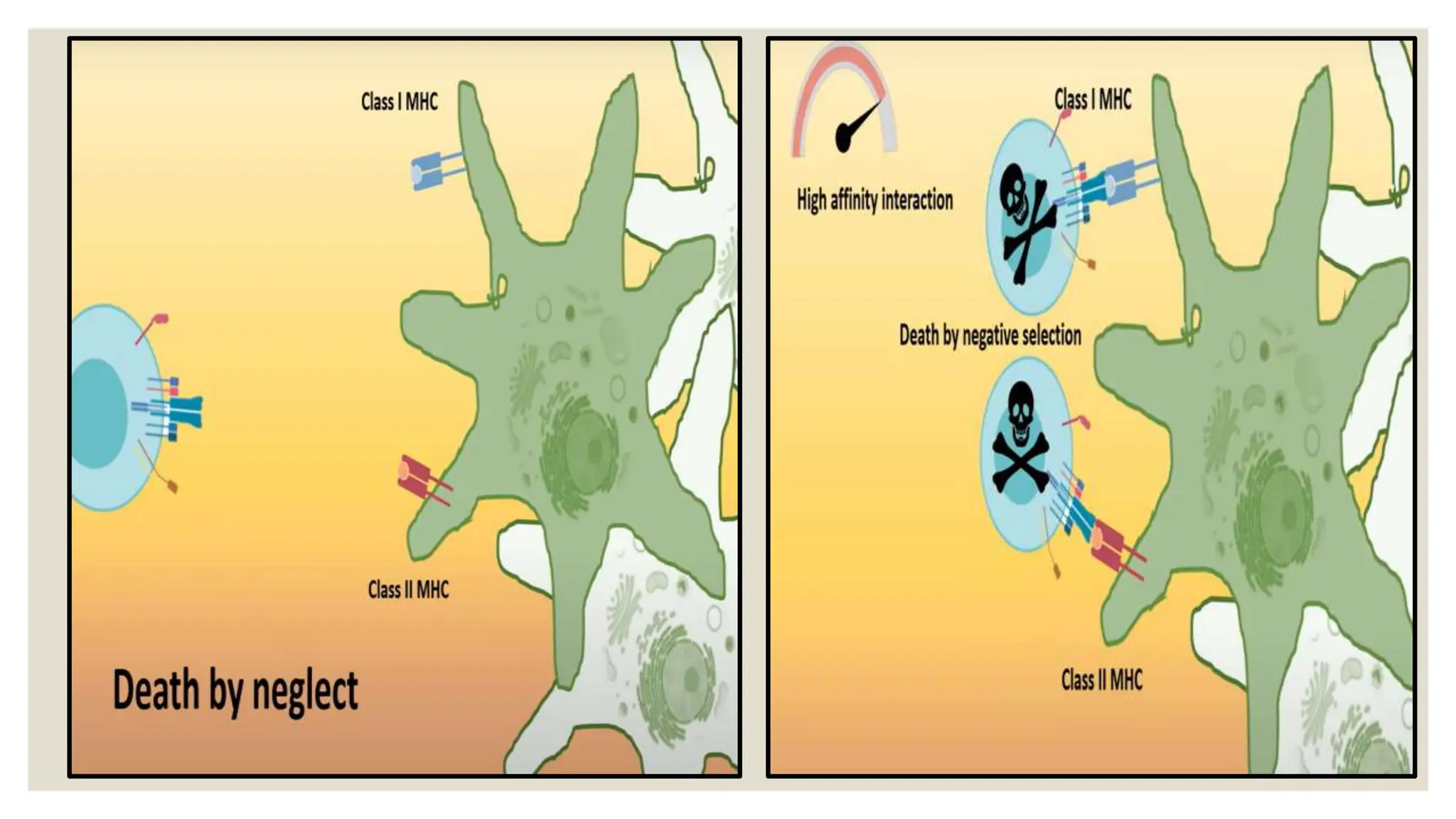
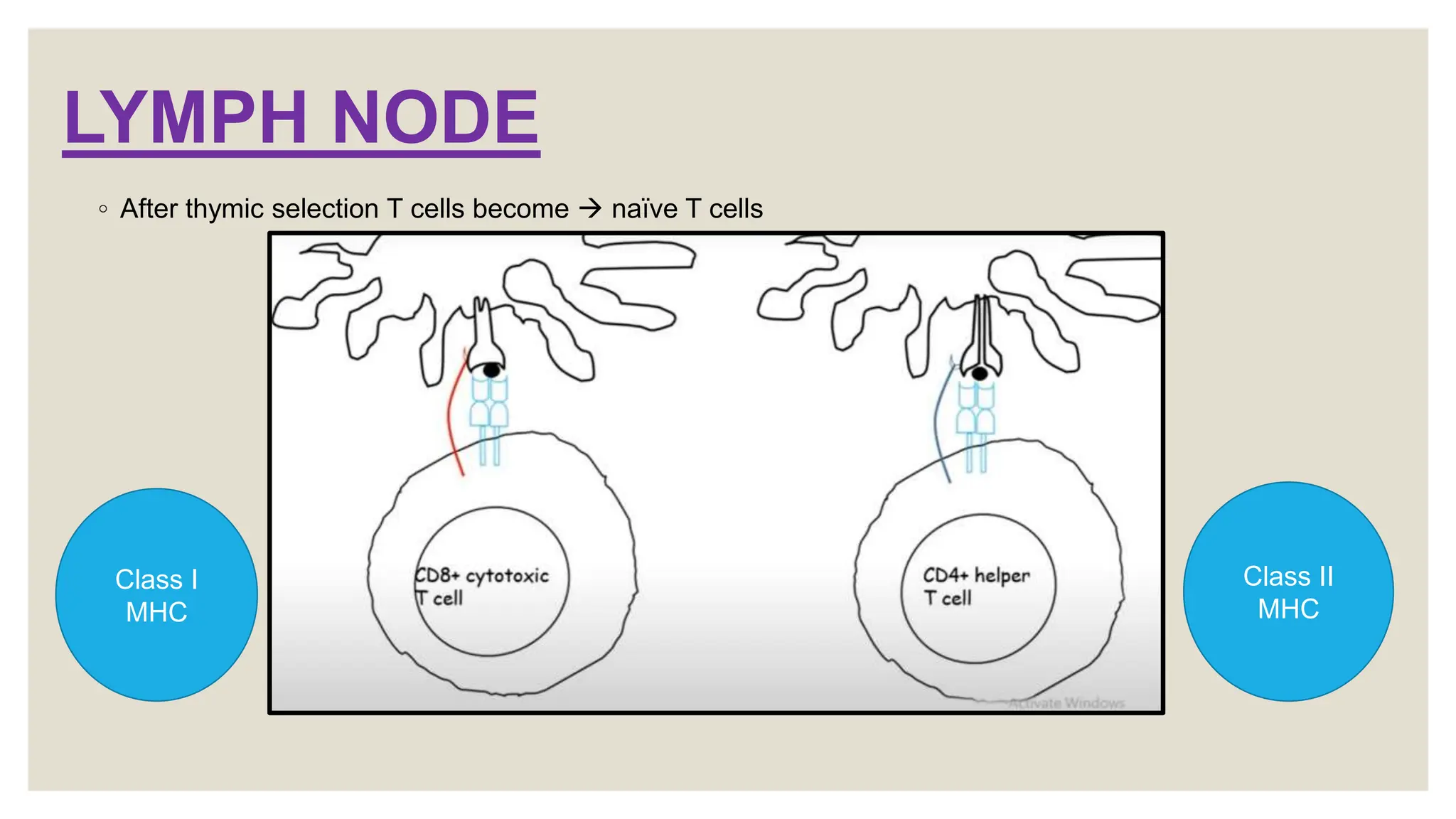
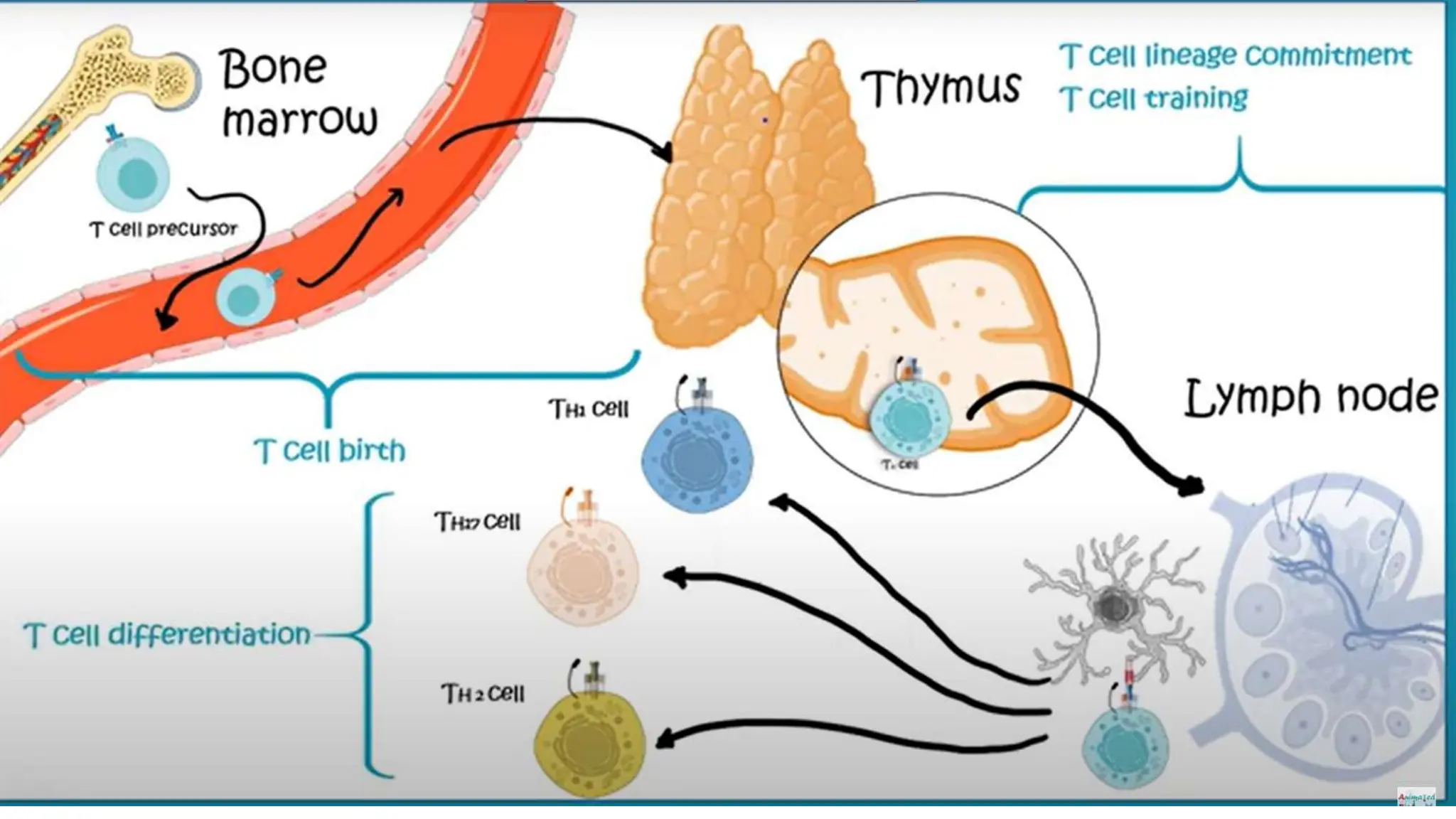
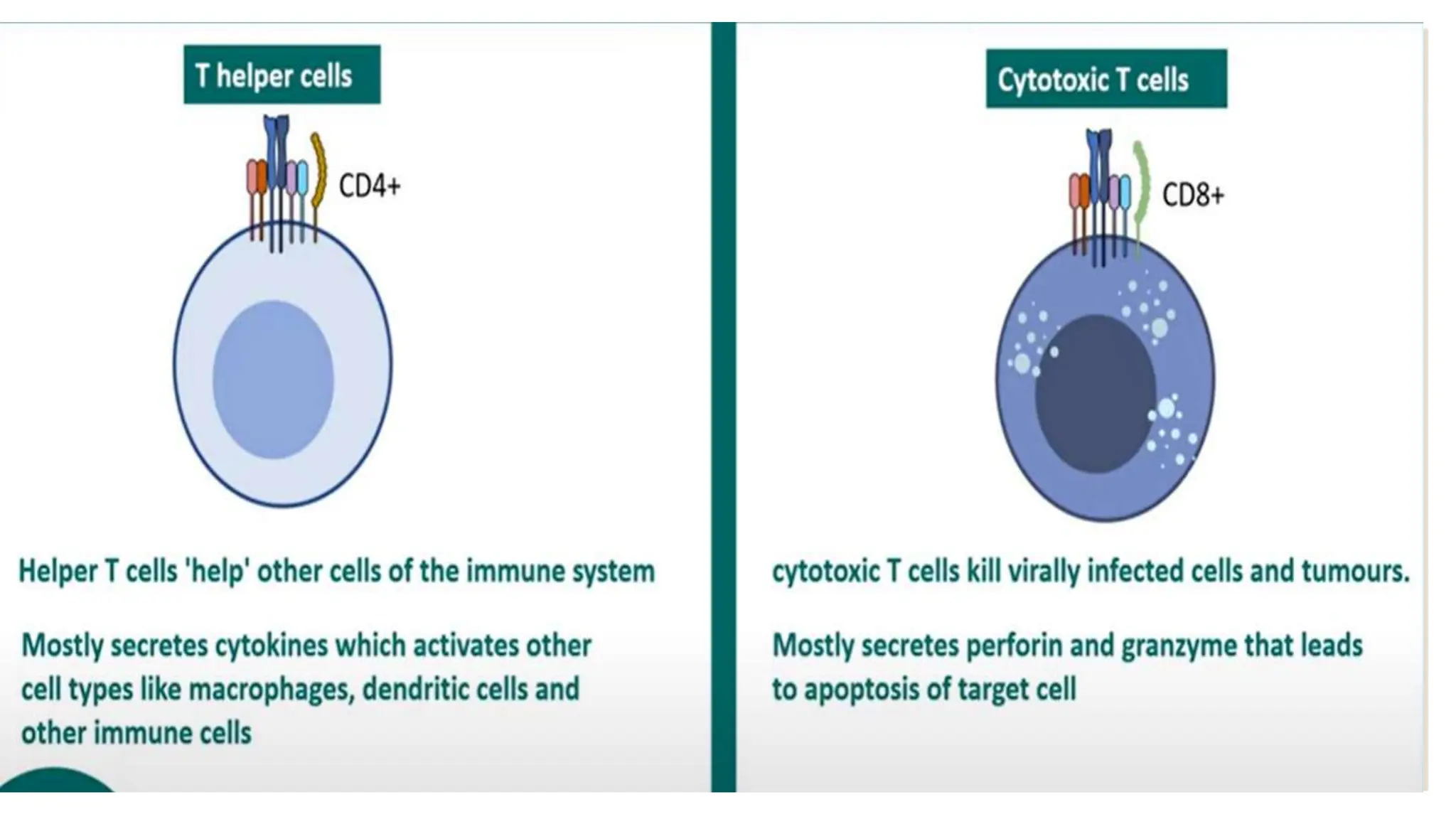
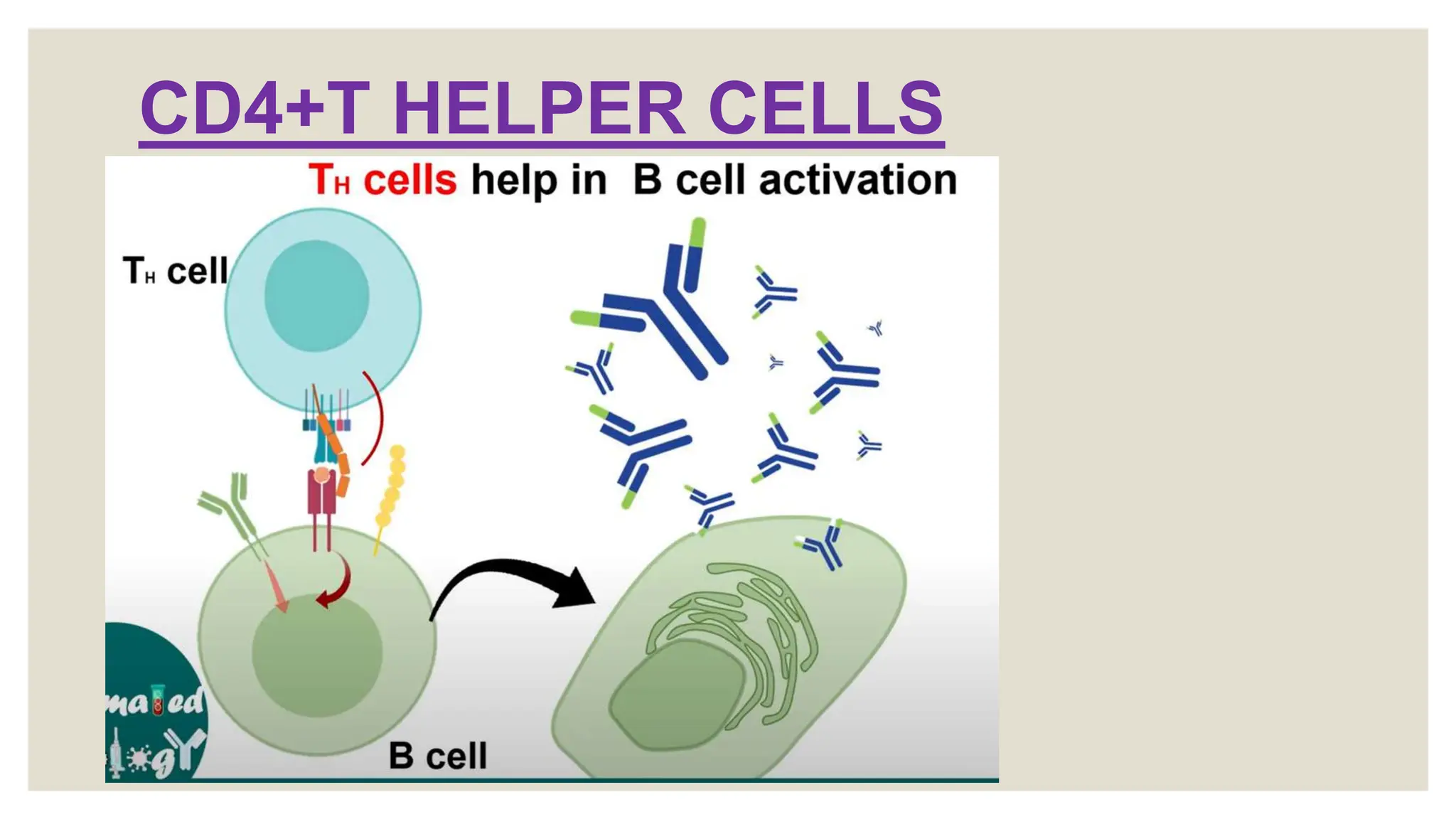
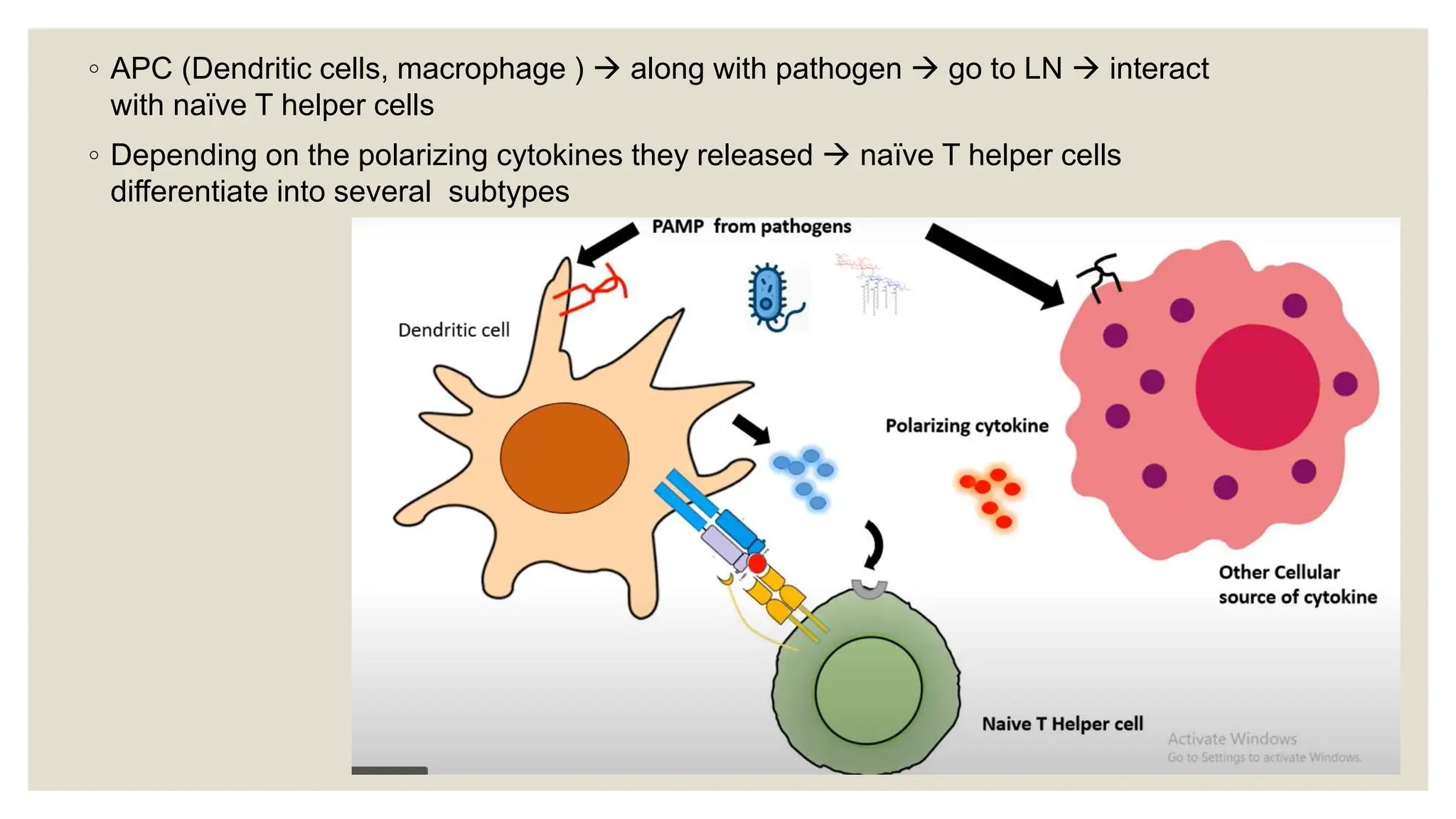
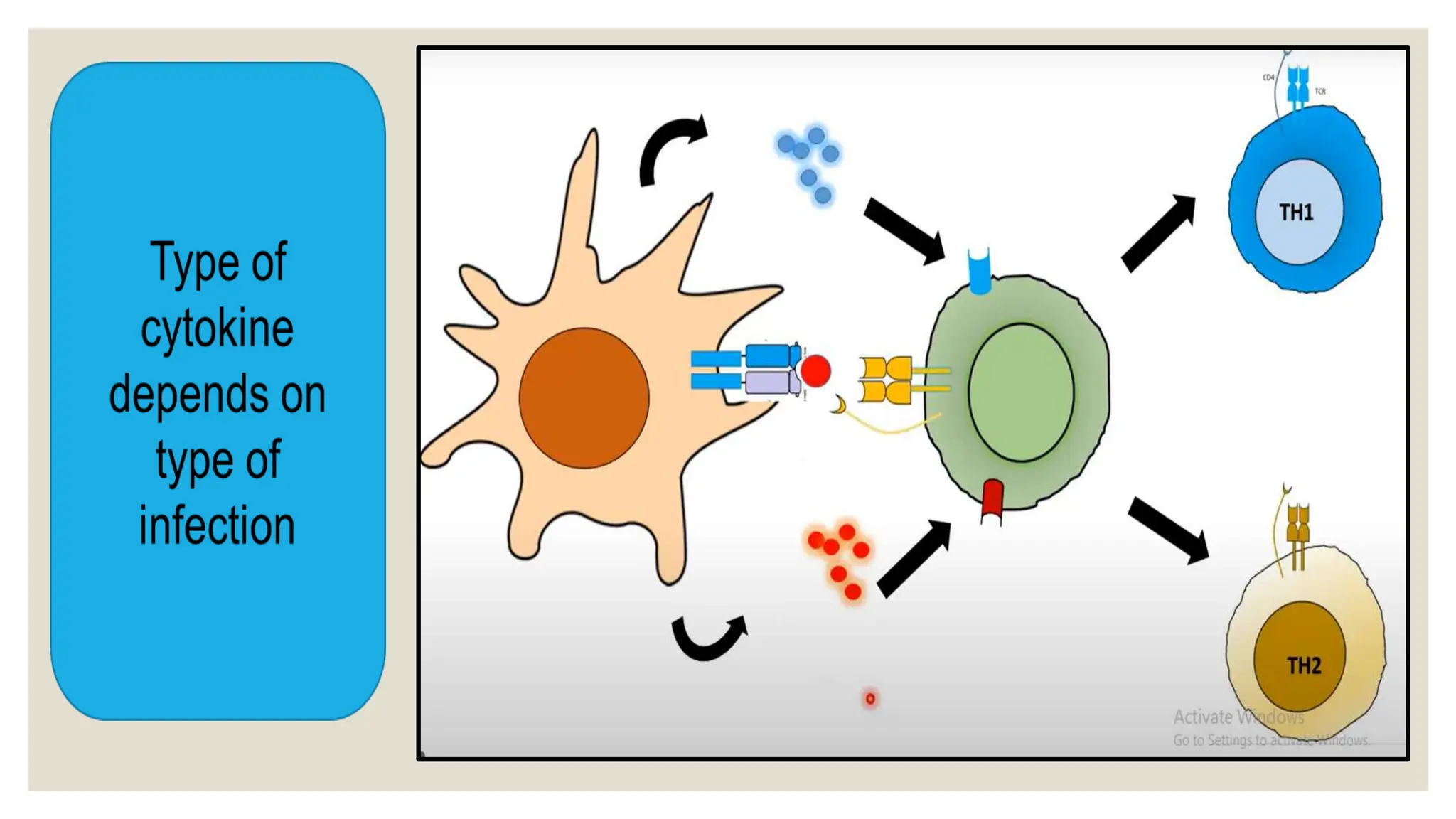
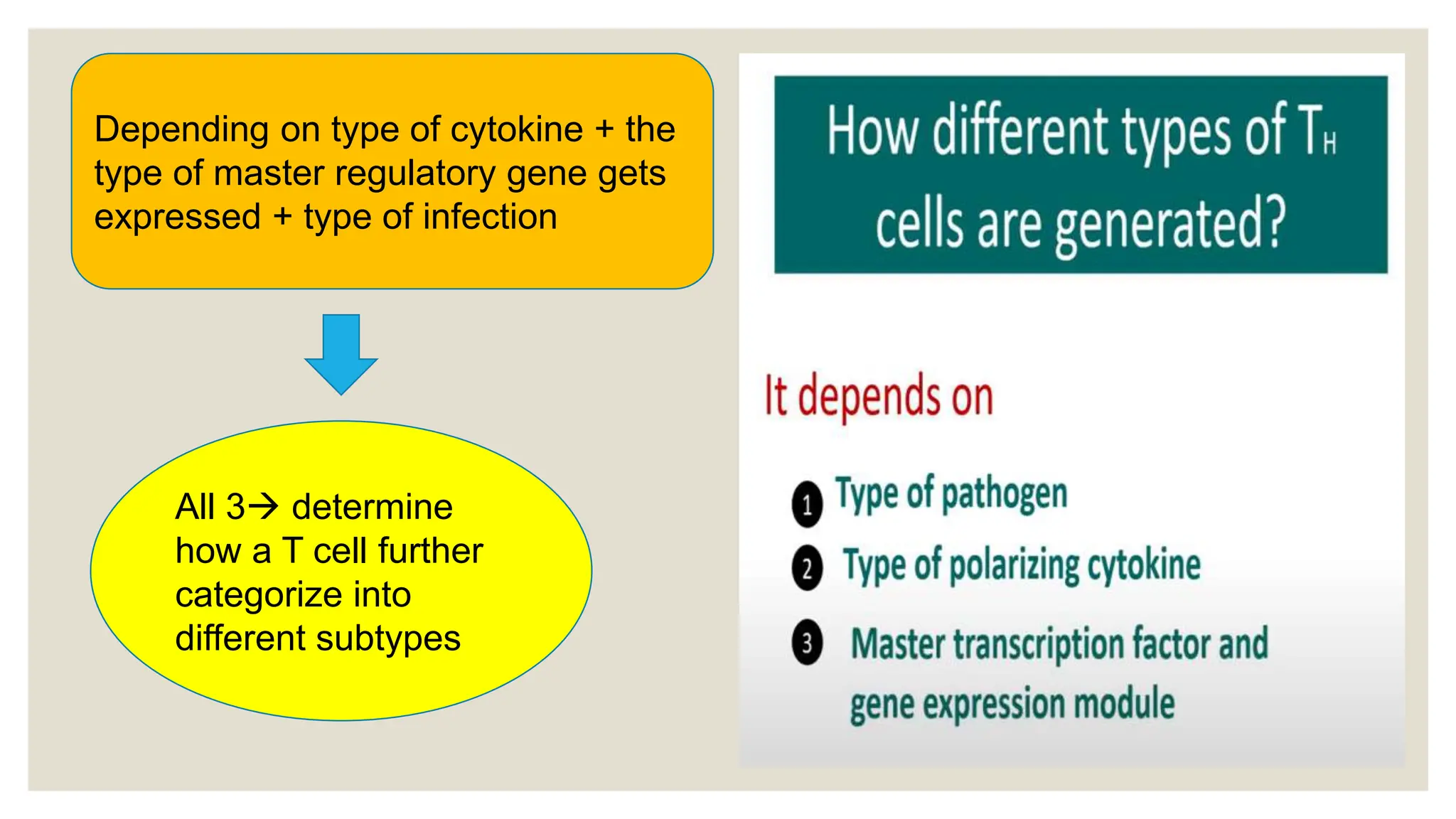
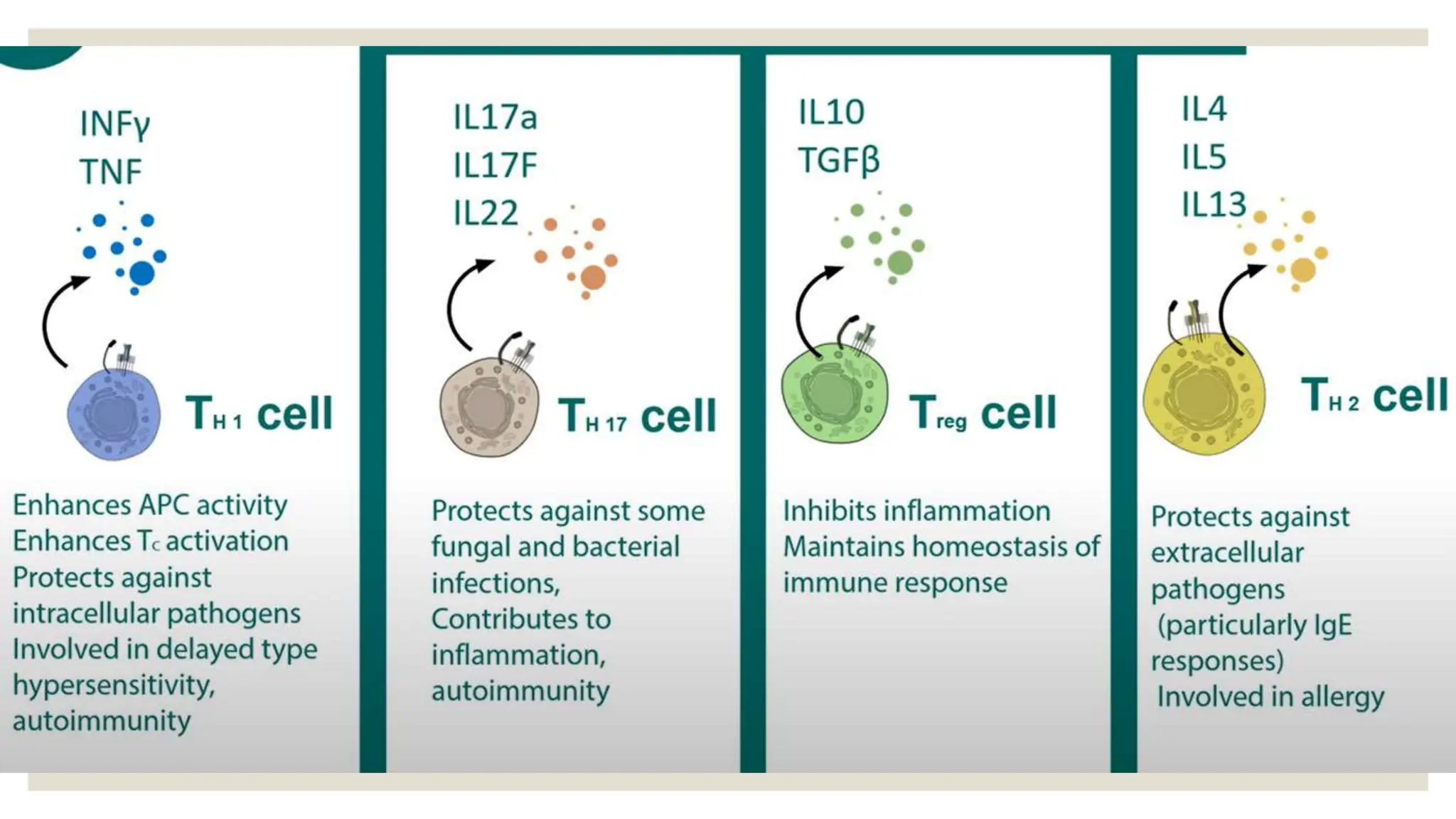
The document outlines the development, maturation, and differentiation of T cells, which are a crucial type of white blood cell involved in immune response. It details the types of T cells, including CD4+ T helper cells, regulatory T cells, CD8+ cytotoxic cells, and memory T cells, as well as the phases of T cell activation. The document also highlights the processes of thymic training and selection, as well as the functions and implications of different T cell subtypes in immune regulation and responses to infection.