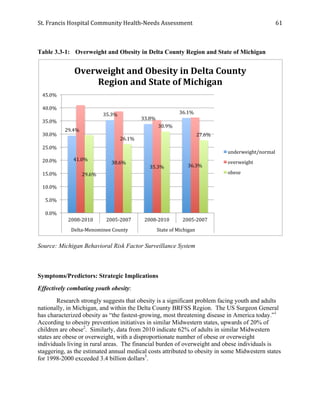
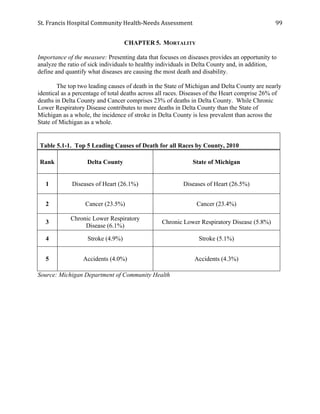
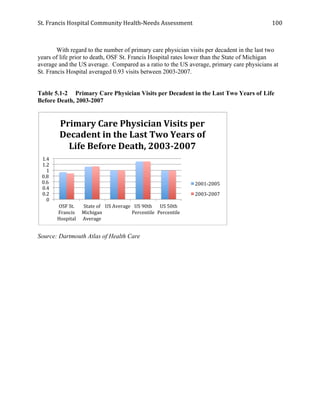
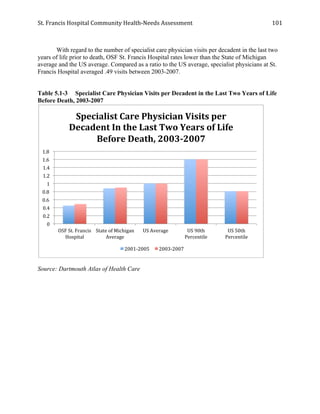
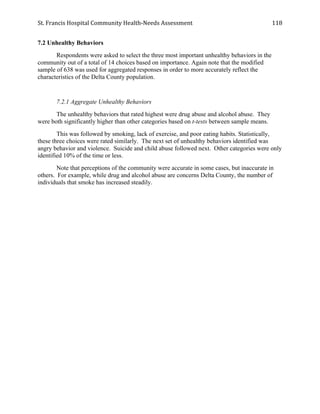
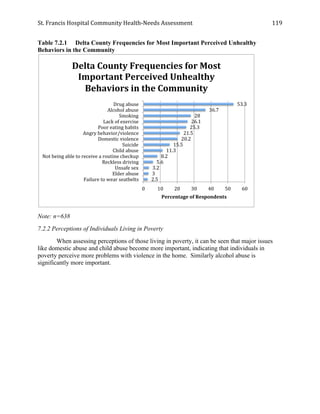
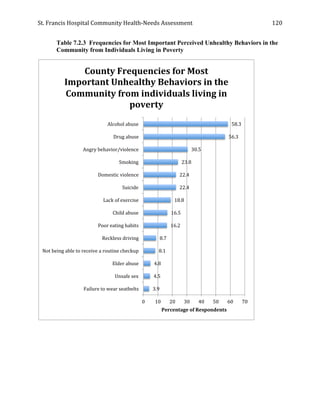
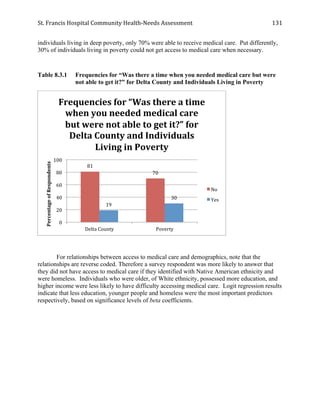
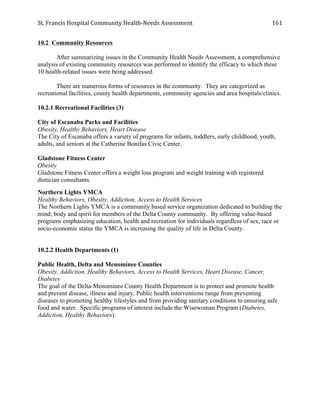
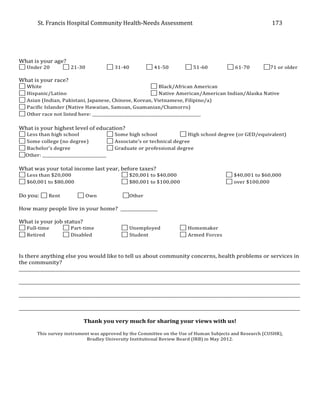
This document provides a community health needs assessment for St. Francis Hospital in Delta County, Michigan. It analyzes demographic data, health behaviors and outcomes, and prioritizes key community health issues. Phase 1 examines demographic profiles, prevention activities, health symptoms/predictors, diseases/morbidity rates and mortality rates. Phase 2 discusses a community survey on health access and behaviors. Phase 3 prioritizes issues like cardiovascular disease, cancer, diabetes, and access to care. Overall, the assessment identifies areas to guide St. Francis' community health improvement strategies and ensure residents have their needs met.