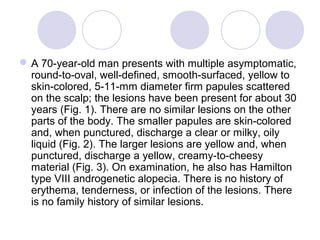
- A 70-year-old man presented with multiple asymptomatic yellow to skin-colored nodules on his scalp that had been present for 30 years.
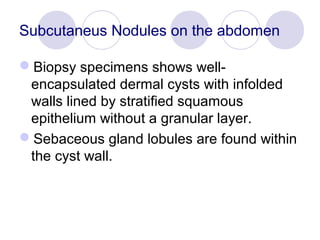
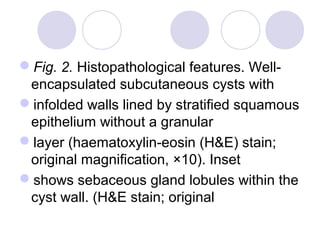
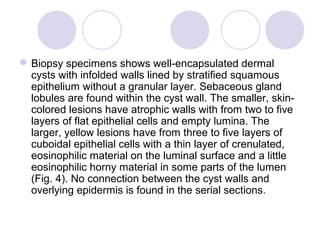
- Biopsy showed well-encapsulated dermal cysts lined with stratified squamous epithelium and sebaceous gland lobules within the cyst wall.
- The pathology findings were consistent with a diagnosis of steatocystoma multiplex, however the lesions were limited only to the scalp rather than a more widespread distribution.
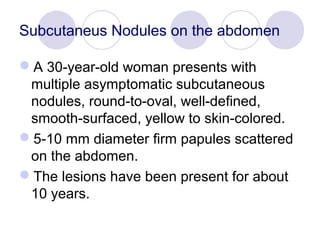


![ In contrast with the typical steatocystoma multiplex patients, lesions are
limited to the scalp in our case. There have been only a few cases with such
a limited distribution [4 6, 9, 10] Table 1 presents a review of the English-
language literature of the published cases of localized forms of
steatocystoma multiplex. In the reported cases of localized steatocystoma
multiplex, the lesions are confined to the head and neck or genitalia. The
terms facial papular variant of steatocystoma multiplex and
sebocystomatosis have been used to describe some of these localized
forms as distinctive variants of the disease [3, 11, 12]. However,
involvement of these areas is not infrequent in typical cases of
steatocystoma multiplex [1]. There are reports of the cases with
steatocystoma multiplex involving predominantly the face or head and neck
with scattered lesions on the trunk [13]. The pathological and clinical
features of the localized forms are not different from typical cases.
Therefore, we believe that the localized forms of steatocystoma multiplex
are not distinctive variants of the disease. Steatocystoma multiplex should
be considered as a spectrum with different variations in anatomical
distribution.](https://image.slidesharecdn.com/subcutaneousnodulesontheabdomen-101026143633-phpapp02/85/Subcutaneous-nodules-on-the-abdomen-13-320.jpg)