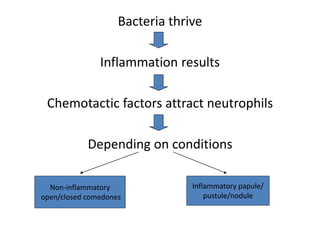
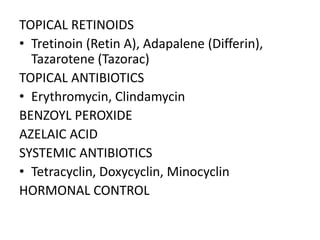
This document defines and describes common paediatric skin lesions. It discusses primary lesions such as macules, papules, vesicles and pustules. It also covers secondary lesions including scaling, lichenification and crusting. The document provides details on the etiology, pathophysiology, clinical features, diagnosis and treatment of common paediatric skin conditions like acne, warts and scabies.