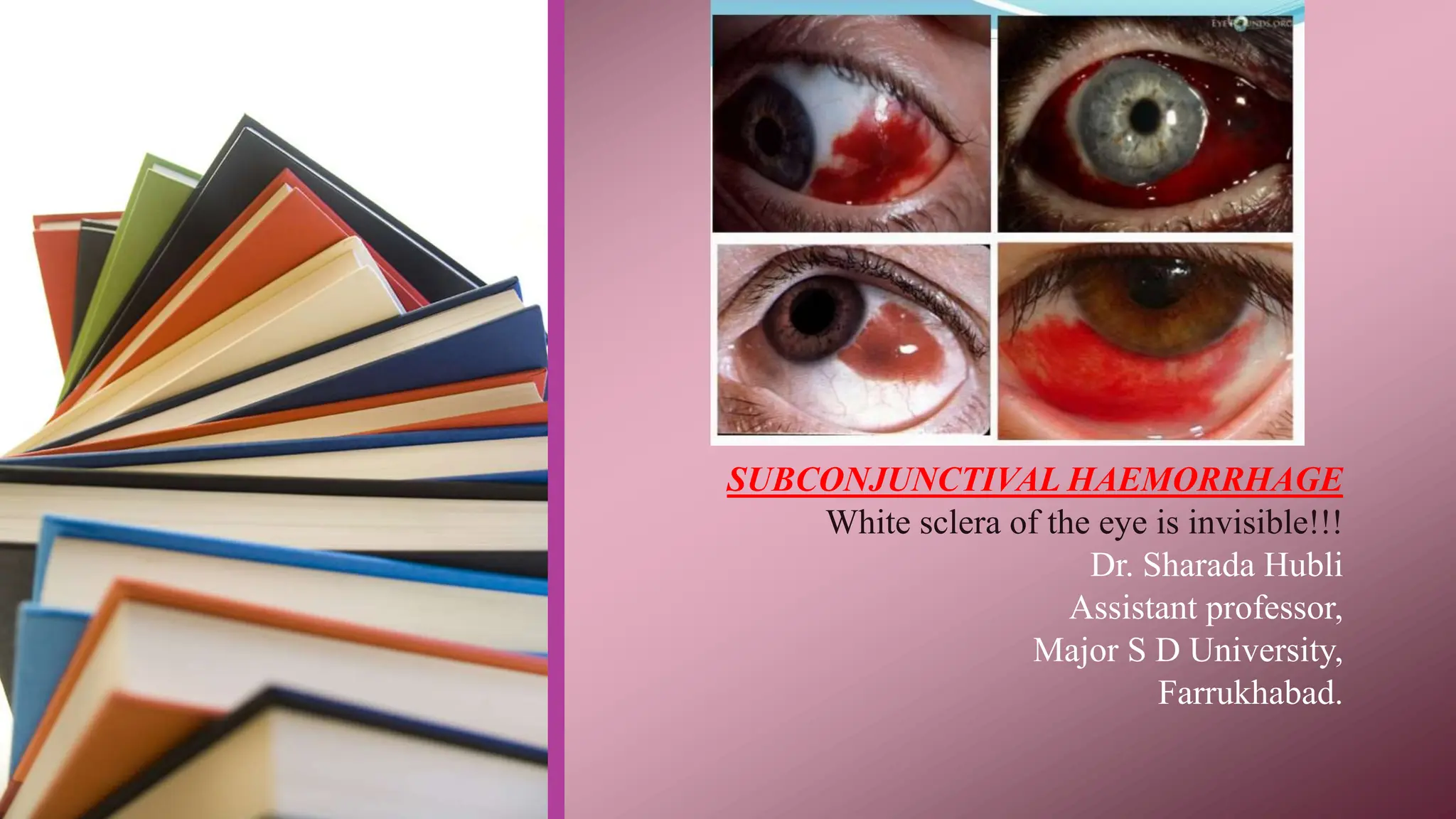
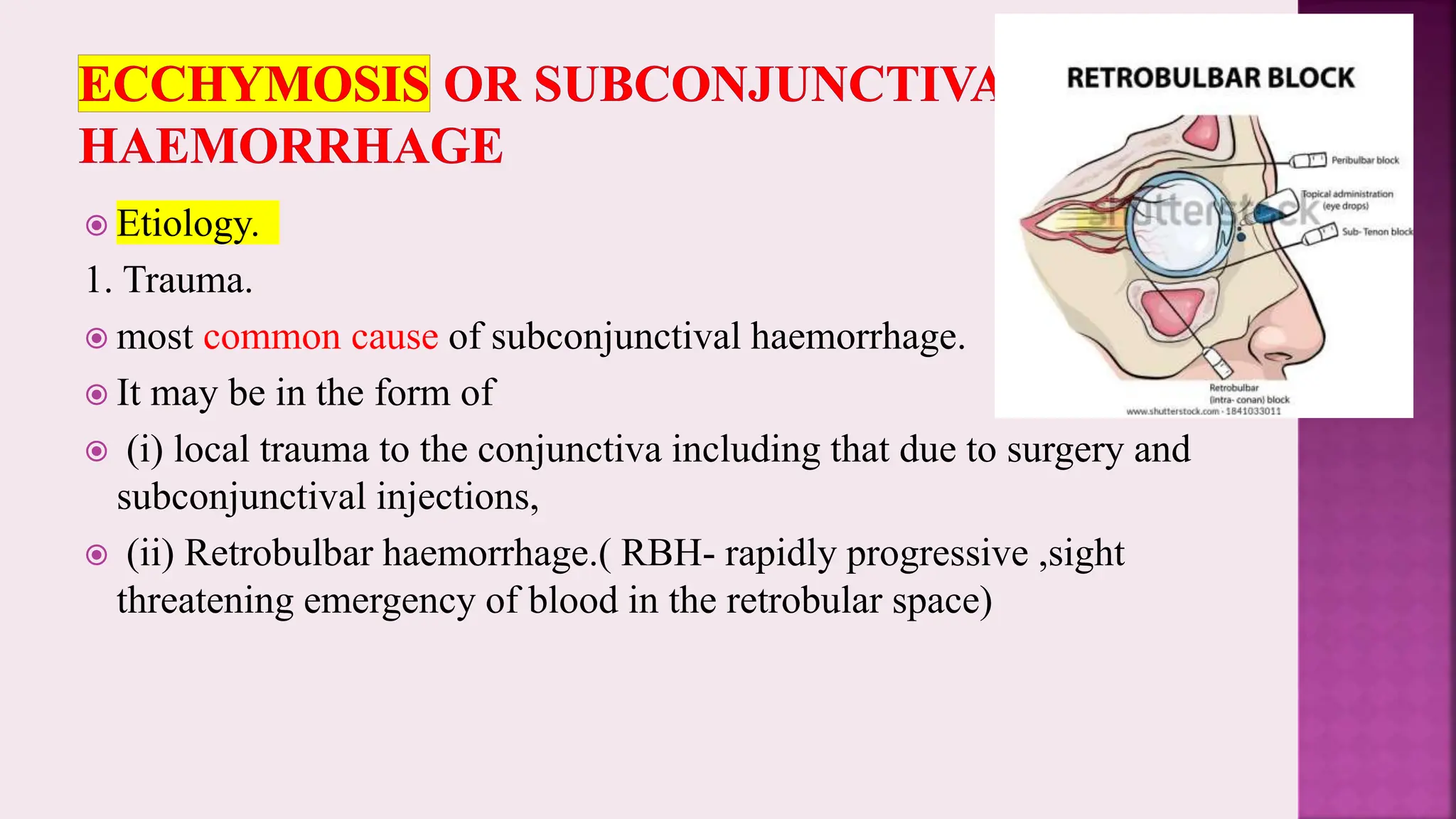
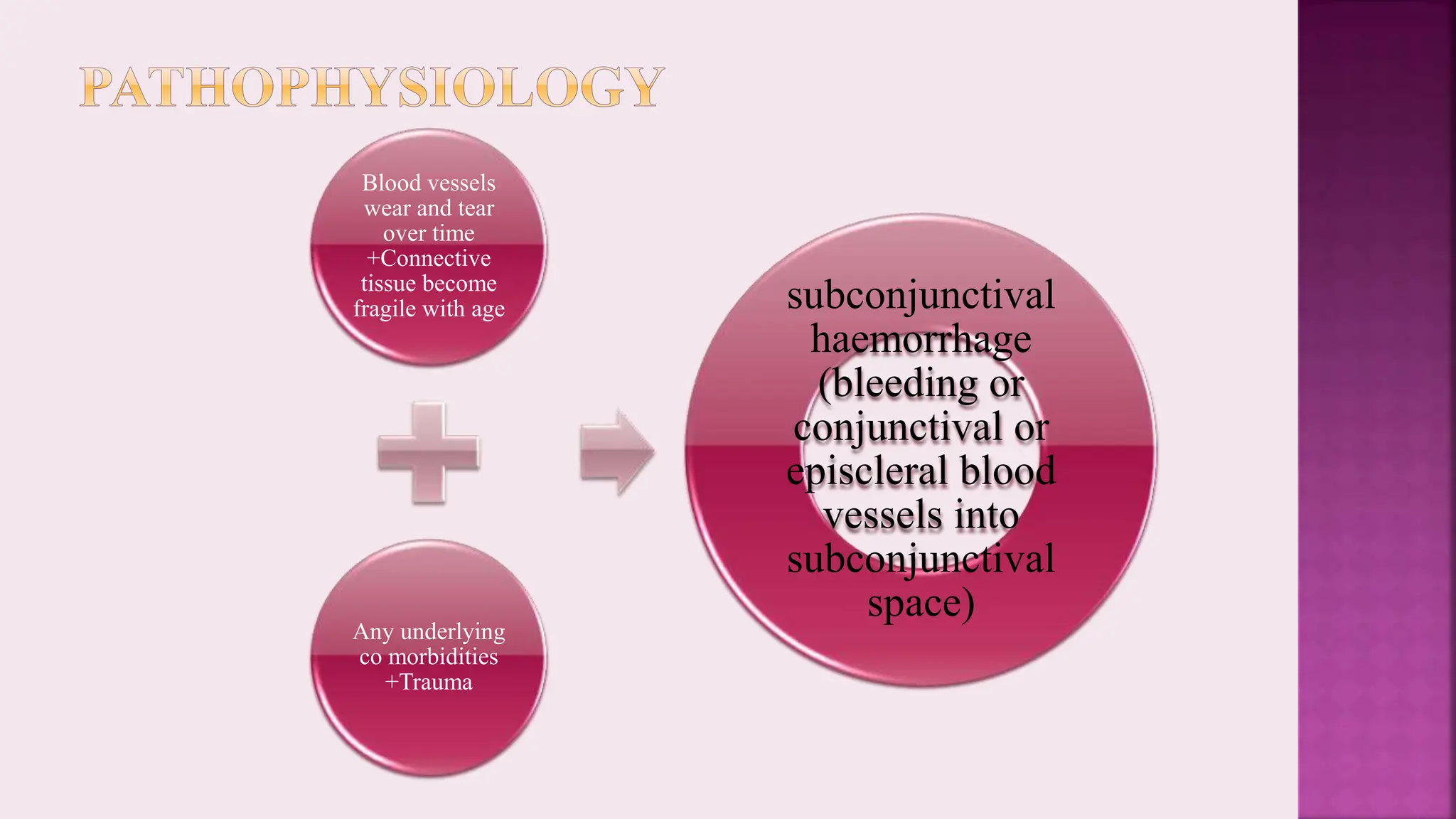
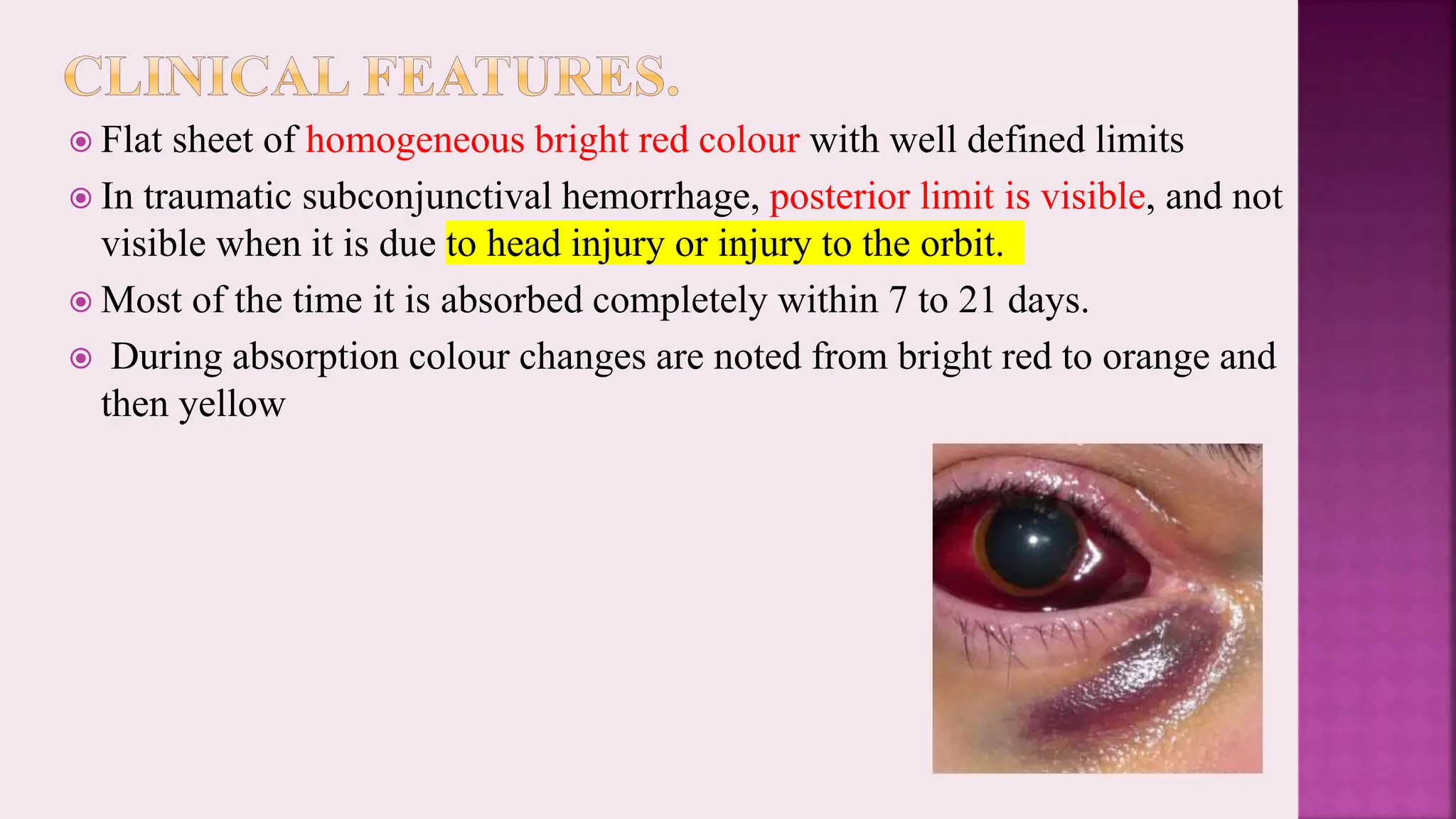
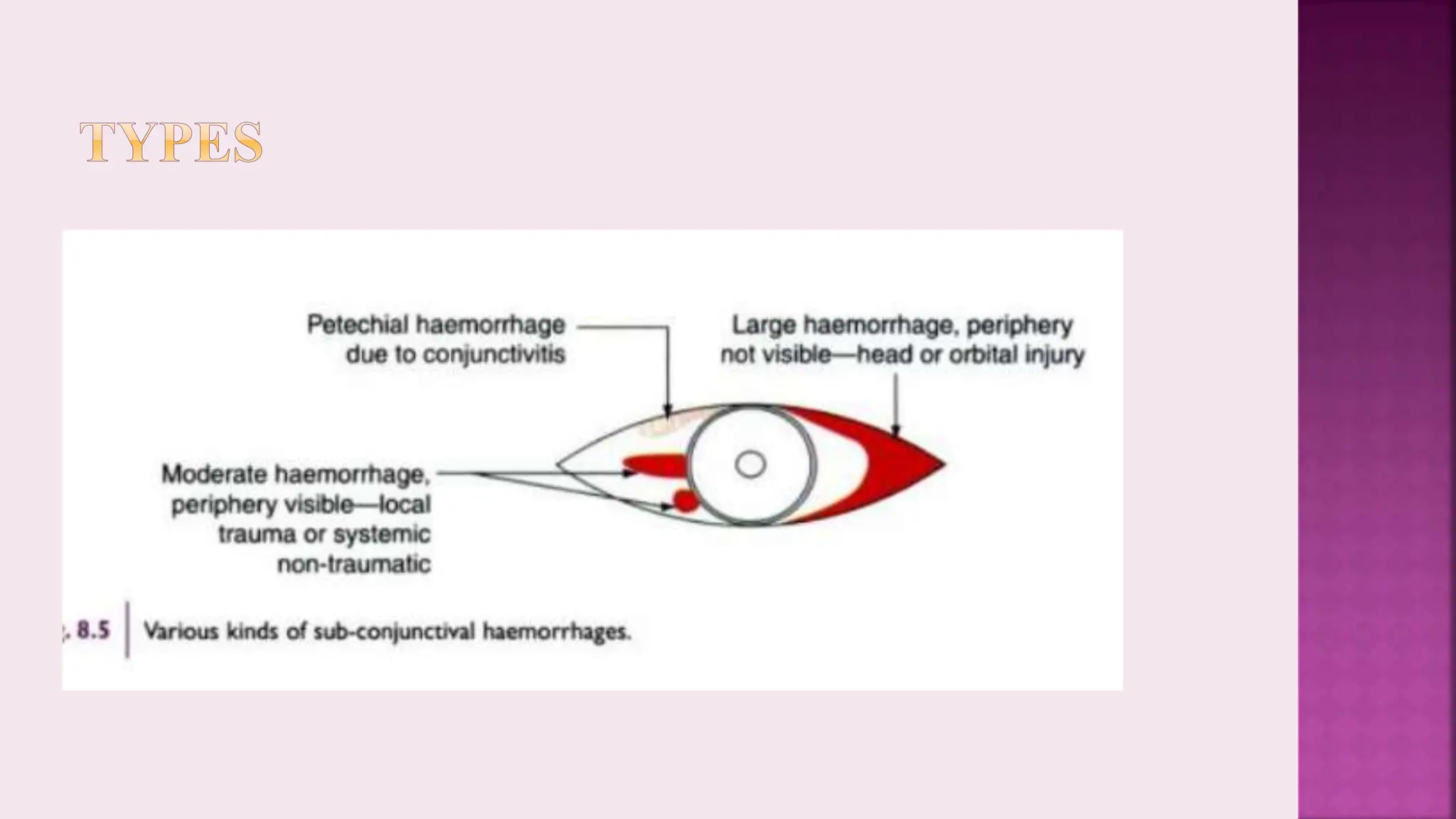
Subconjunctival hemorrhage results in the temporary obscuring of the white sclera of the eye, which can range from minor bleeding to extensive discoloration. The condition can arise from various causes, including trauma, inflammation, venous congestion, vascular diseases, bleeding disorders, and certain infections. Most cases resolve on their own within 7 to 21 days; treatment focuses on addressing the underlying cause and providing patient reassurance.