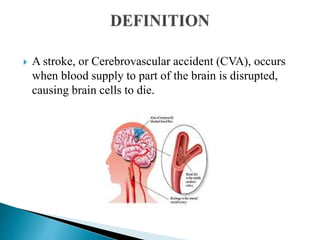
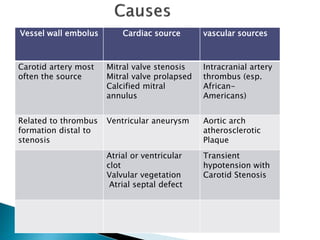
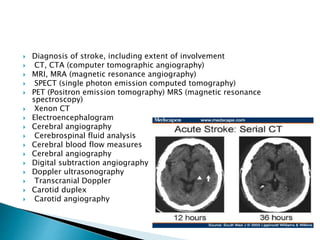
The document provides an overview of cerebrovascular disorders, particularly focusing on strokes, which occur due to disrupted blood supply to the brain. It details risk factors, types of strokes, symptoms, diagnostic methods, and treatment options, including antiplatelet and thrombolytic therapies. Additionally, it emphasizes the importance of assessing cognitive and motor functions in stroke patients.













![ Platelet-inhibiting medications: Aspirin,
dipyridamole [Persantine], clopidogrel
[Plavix], and ticlopidine [Ticlid]). Currently the
most cost-effective antiplatelet regimen is
aspirin 50 mg/d and dipyridamole 400 mg/d.
Thrombolytic therapy: Recombinant t-PA is a
genetically engineered form of t PA, a
thrombolytic substance made naturally by the
body. The minimum dose is 0.9 mg/kg; the
maximum dose is 90 mg](https://image.slidesharecdn.com/cvamalarmathim-221220061822-6012b083/85/CVA-MALARMATHI-M-pptx-18-320.jpg)




