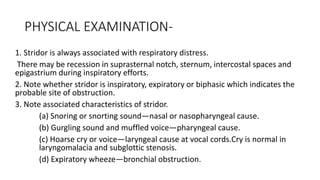
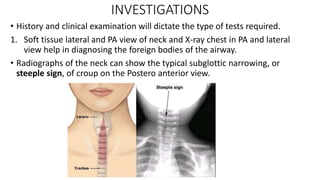
1. Stridor requires determining the cause through history and physical exam including timing, onset, associated symptoms, and localization of obstruction.
2. Flexible fiberoptic laryngoscopy can diagnose conditions like laryngomalacia by examining the nose, throat, and larynx without general anesthesia.
3. Treatment depends on the diagnosed cause, such as racemic epinephrine, dexamethasone, or antibiotics for croup, immediate intubation and antibiotics for epiglottitis, and bronchoscopy for removing foreign bodies.