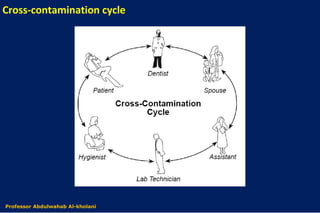
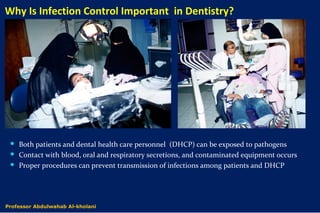
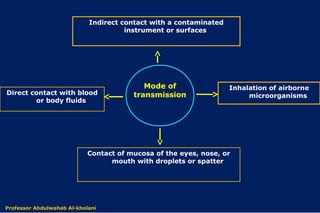
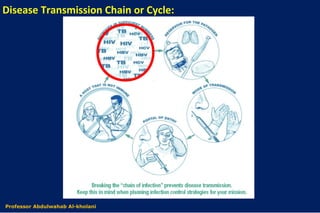
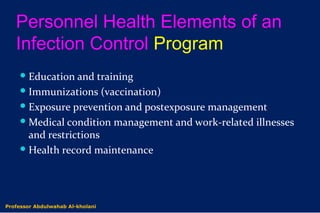
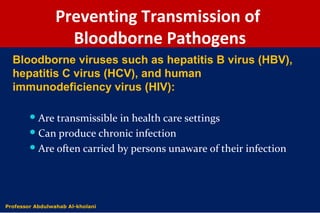
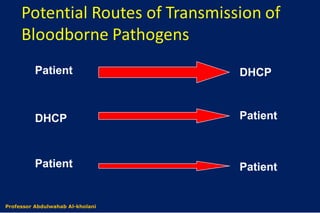
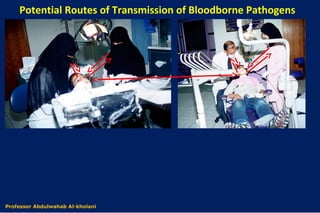
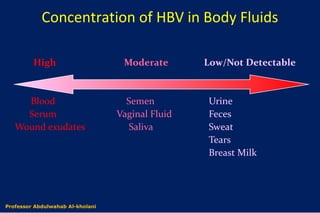
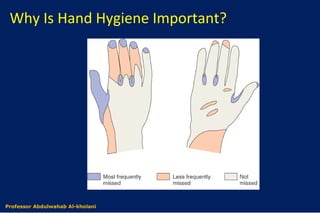
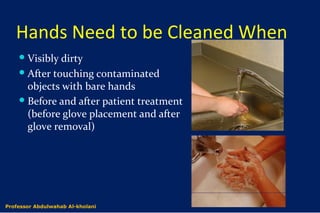
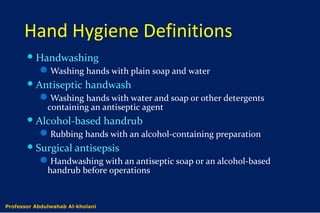
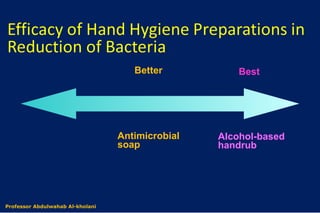
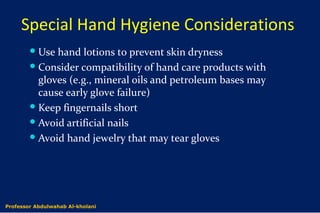
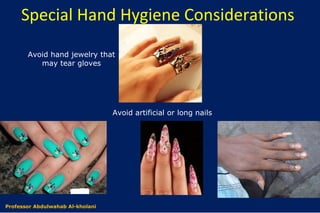
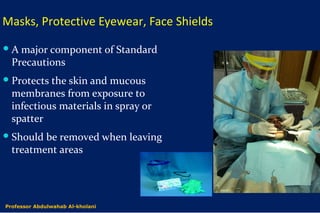
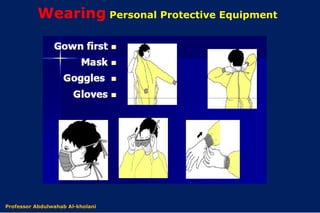
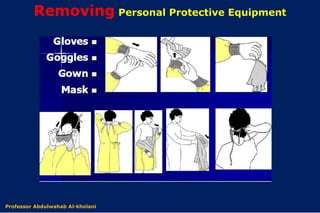
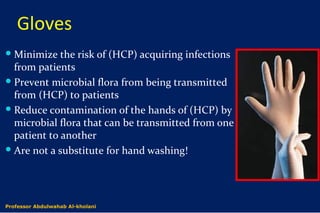
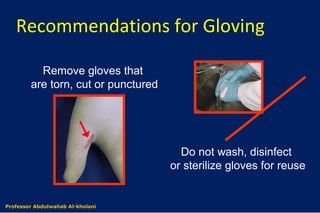
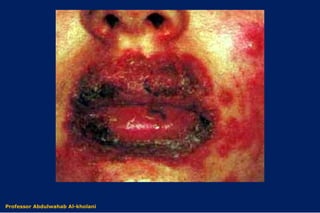
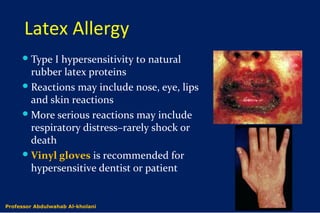
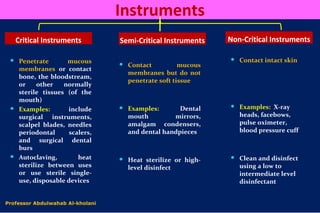
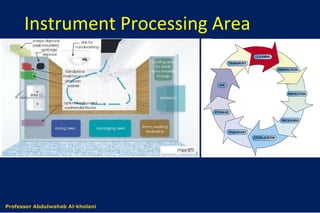
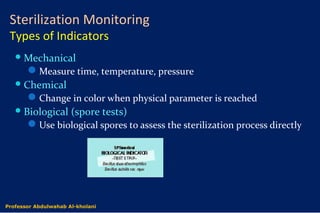
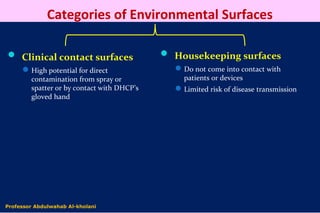
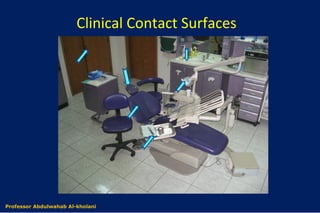
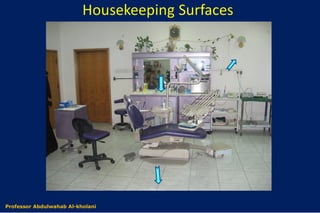
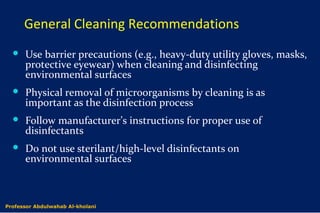
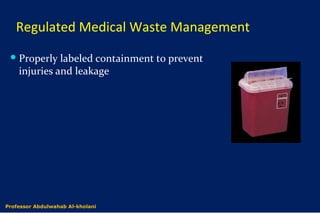
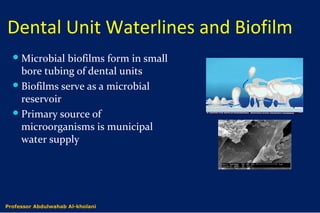
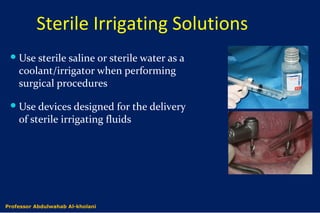
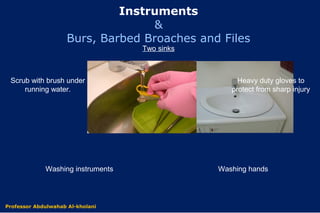
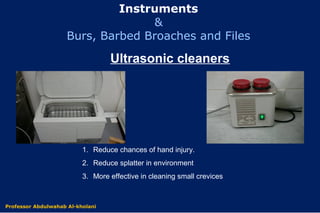
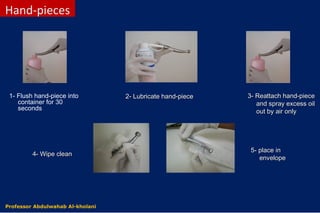
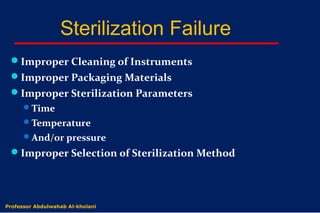
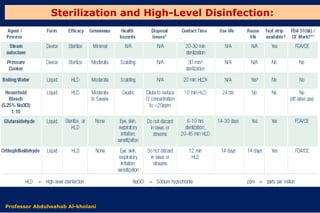
The document outlines essential infection control practices in dentistry, emphasizing the importance of preventing the transmission of pathogens through proper procedures like hand hygiene, sterilization, and the use of personal protective equipment (PPE). It details modes of disease transmission, personnel health considerations, and the significance of maintaining sterile environments and instrument processing. Additionally, it addresses biofilm management in dental unit waterlines and provides specific recommendations for managing medical waste.