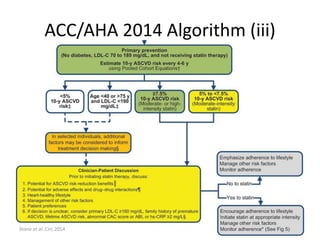
- The document discusses guidelines for statin use in primary prevention from the 2014 ACC/AHA, including algorithms for determining statin eligibility based on estimated 10-year risk of atherosclerotic cardiovascular disease (ASCVD).
- It notes that the guidelines lower the risk threshold for statin recommendation from greater than 7.5% 10-year ASCVD risk to greater than 5% for some patients.
- Concerns raised about the guidelines include the selection of studies included in reviews and the lack of consideration of observational data or post-hoc analyses of randomized controlled trials.


![A Tale Of Two Types of Endpoints
• The term “surrogate marker” dates from the late
1980s, but it had been preceded by the term
“biomarker” and was succeeded and replaced by
yet another term, “surrogate endpoint”.
• A surrogate endpoint has been defined as “a
biomarker intended to substitute for a clinical
endpoint”
• A clinical [hard] endpoint is “a characteristic or
variable that reflects how a patient feels,
functions, or survives”
Brotman&Prince Vox Sang 1988; Paone et al. J Surg Oncol 1980; Boone&Kelloff J Cell Biochem Suppl 1993; NIH Definitions
Working Group. Biomarkers and Surrogate Endpoints. 2000. Cited after Aronson Br J Pharmacol 2005](https://image.slidesharecdn.com/statinwars-141111143844-conversion-gate02/85/Statin-Wars-4-320.jpg)