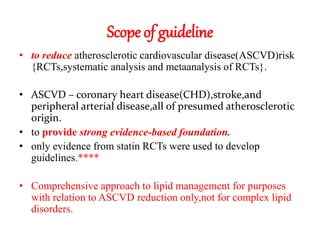
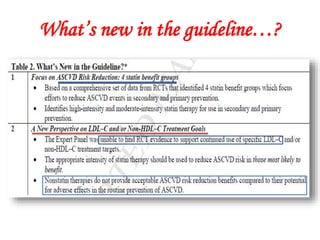
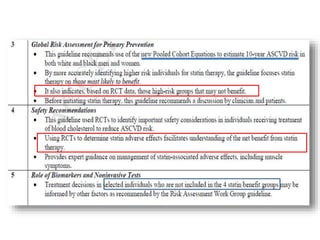
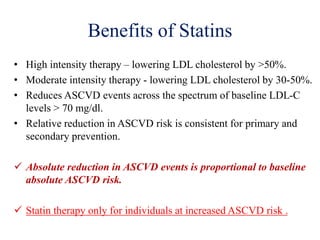
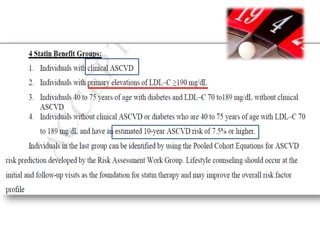
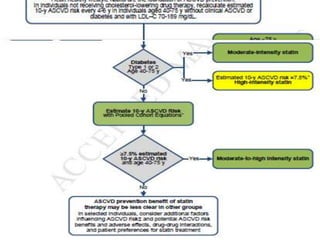
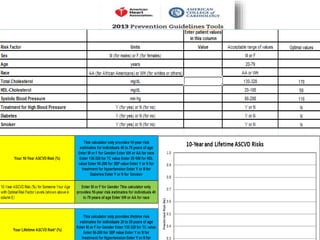
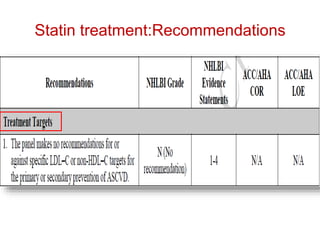
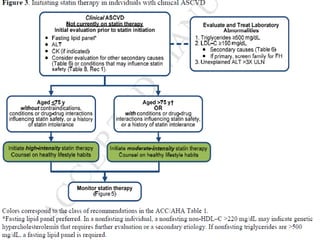
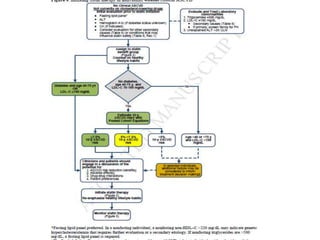
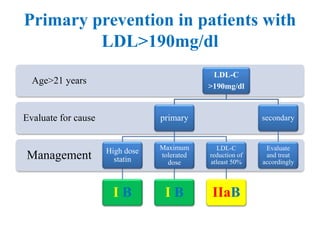
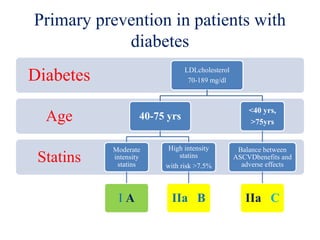
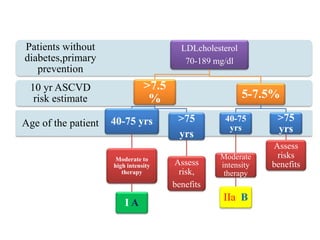
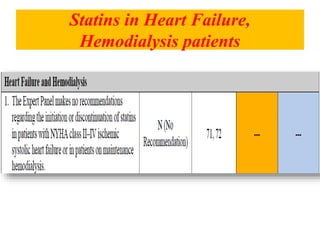
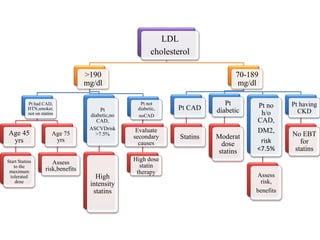
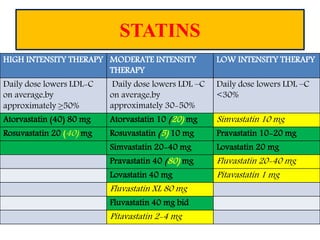
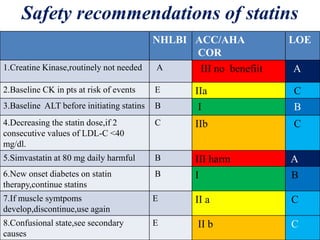
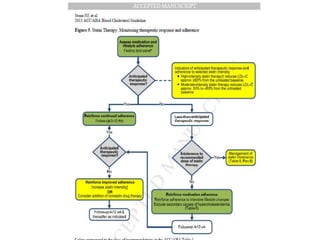
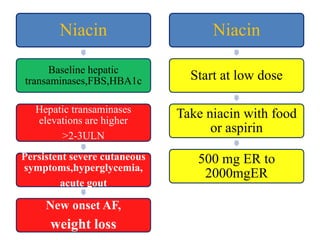
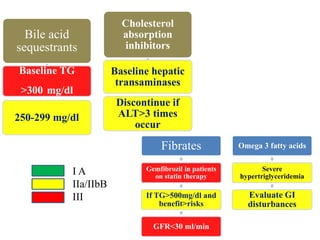
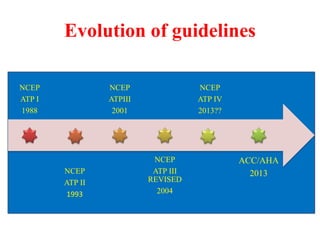
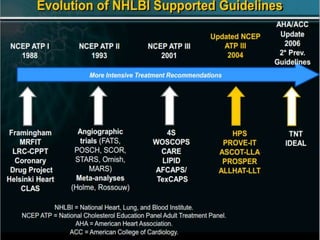
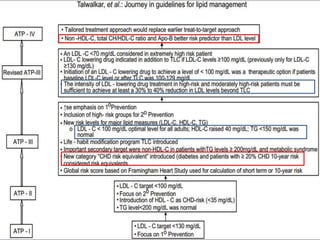
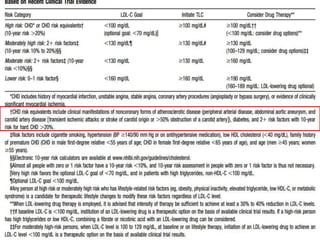
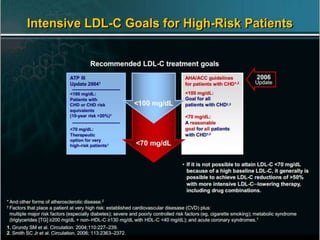
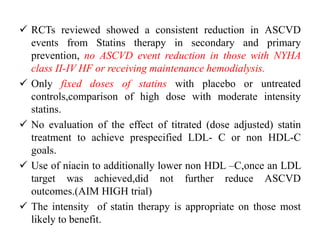
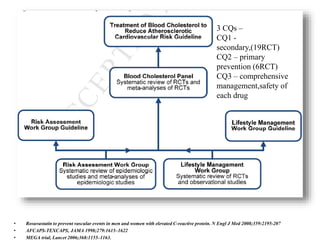
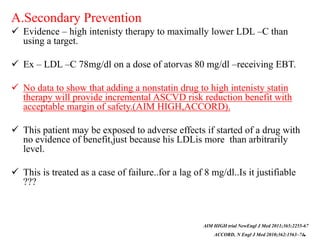
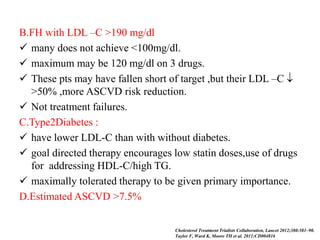
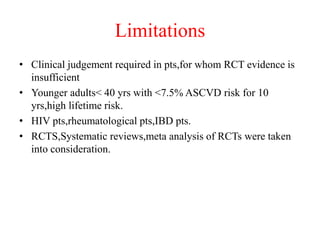
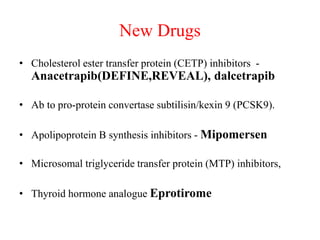
The document summarizes the 2013 ACC/AHA blood cholesterol treatment guidelines. The guidelines aim to reduce atherosclerotic cardiovascular disease risk based on evidence from statin randomized controlled trials. The guidelines recommend a patient-centered approach and emphasize that high- and moderate-intensity statin therapy provides the greatest reduction in risk across all baseline LDL-C levels. Primary prevention recommendations are based on estimated 10-year cardiovascular risk. The guidelines do not recommend targeting specific LDL-C levels but rather emphasize intensity of statin therapy.