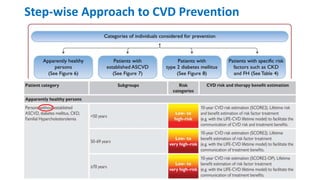
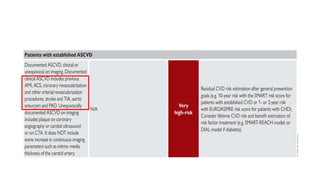
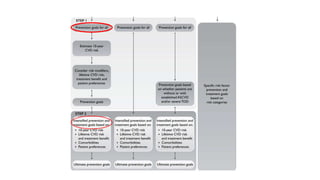
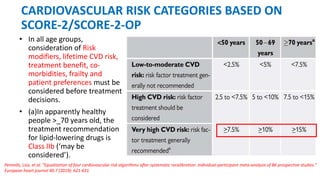
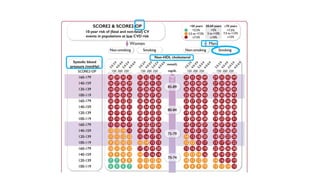
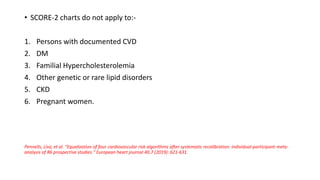
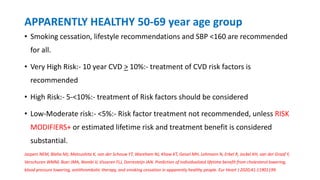
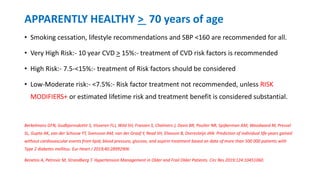
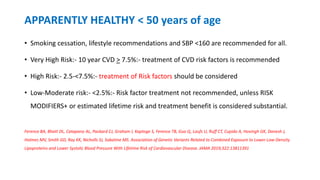
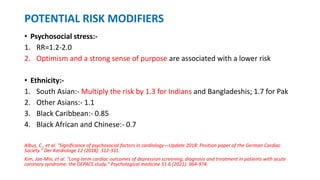
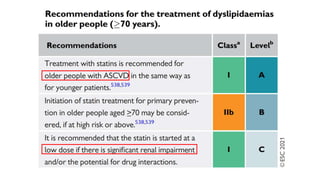
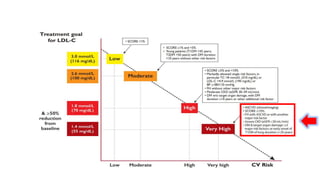
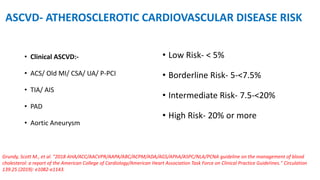
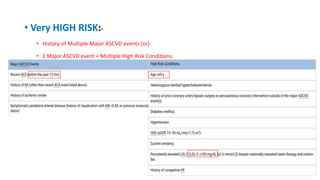
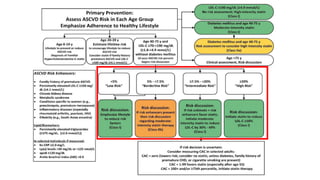
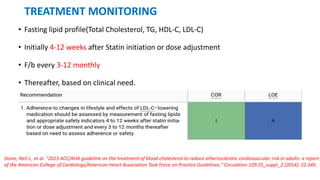
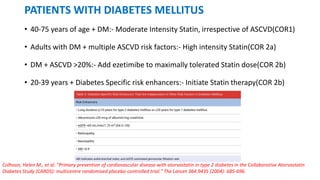
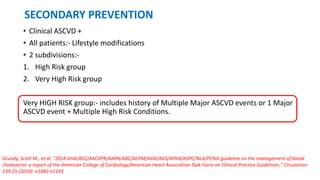
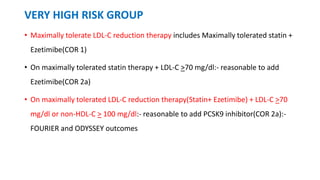
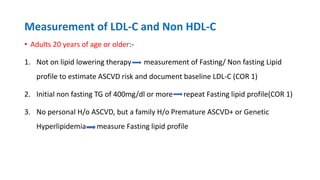
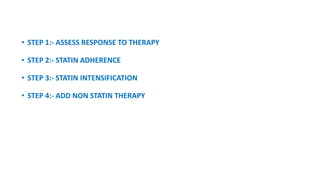
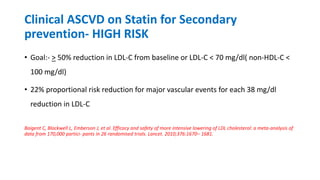
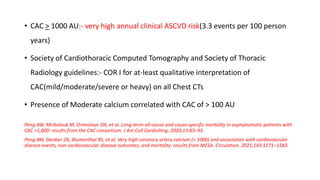
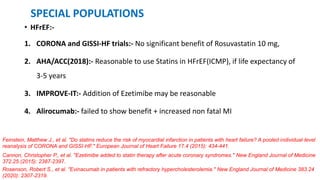
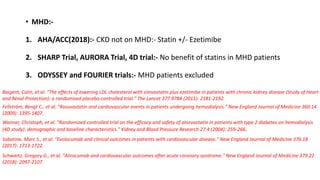
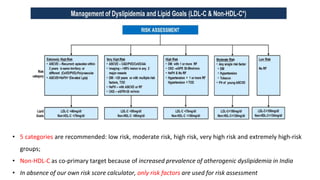
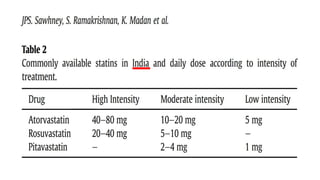
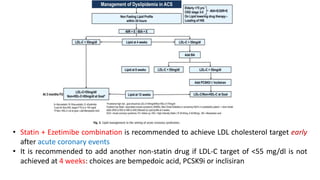
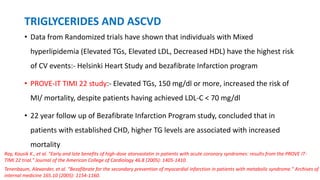
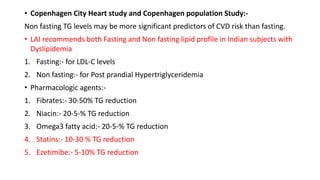
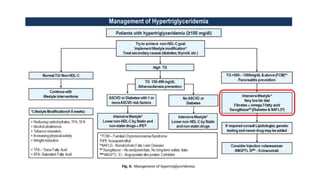
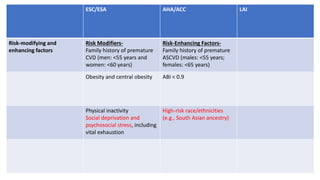
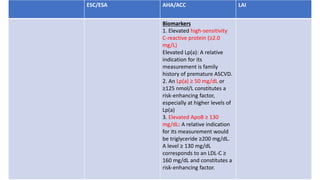
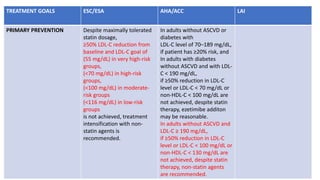
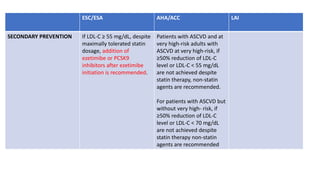
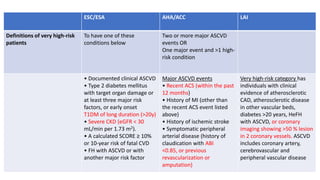
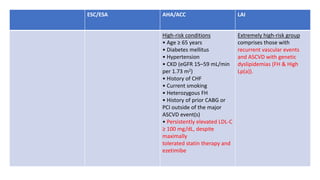
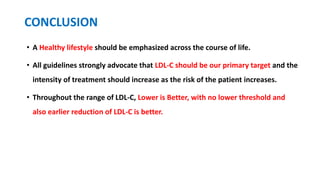
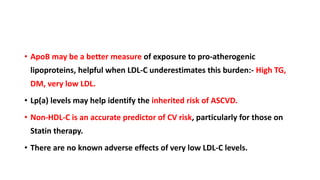
The document presents an overview of the latest lipid guidelines from various organizations, highlighting the role of LDL cholesterol in cardiovascular disease (CVD) risk. It discusses cholesterol treatment strategies, risk classification algorithms, and emphasizes the importance of lifestyle modifications and personalized treatment approaches based on age and risk factors. Additionally, it outlines recommendations for management in different population groups, including older adults and patients with diabetes.