1. Dyslipidemia is an important risk factor for cardiovascular disease and is defined by disorders of lipoprotein metabolism that result in high cholesterol, LDL, and triglycerides or low HDL.
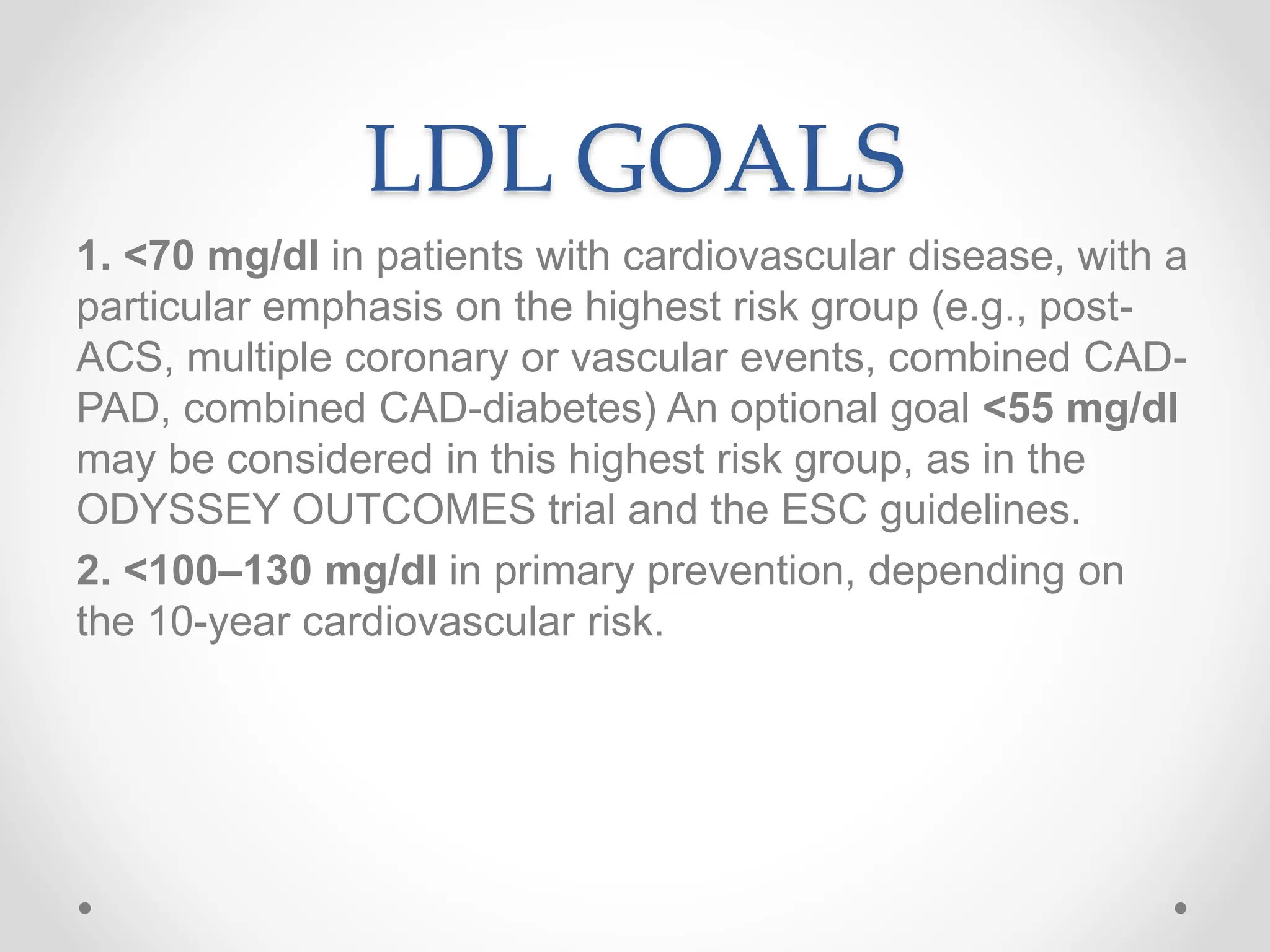
2. Lifestyle changes and medications like statins are recommended to lower LDL levels and reduce cardiovascular risk, with lower LDL targets for those at highest risk.
3. Statins are the first-line treatment for lowering LDL but can cause side effects like muscle pain; newer drugs like PCSK9 inhibitors can further lower LDL in those unable to tolerate statins.
























![Recommendations for Primary Severe Hypercholesterolemia
(LDL-C >190 mg/dl [>4.9 mmol/L])
Class 1 Recommendation
In patients 20 to 75 years of age with an LDL-C level of
190 mg/dl or higher (‡4.9 mmol/L) maximally tolerated
statin therapy is recommended
Class 2a Recommendation
In patients 20 to 75 years of age with an LDL-C level of 190
mg/dl or higher (‡4.9 mmol/L) who achieve less than a 50%
reduction in LDL-C while receiving maximally tolerated
statin therapy and/or have an LDL-C level of 100 mg/dL or
higher (‡2.6 mmol/L) ezetimibe therapy is reasonable](https://image.slidesharecdn.com/dyslipidemiapresentation-231007141849-8eed9ada/75/Dyslipidemia-presentation-pptx-26-2048.jpg)





![Recommendations for Hypertriglyceridemia
• Class 1 Recommendations
In adults 20 years of age or older with moderate
hypertriglyceridemia (fasting or nonfasting triglycerides 175-499
mg/dL [2.0-5.6 mmol/L]), clinicians should address and treat
Lifestyle factors (obesity and metabolic syndrome),
Secondary factors
diabetes mellitus
chronic liver or kidney disease
nephrotic syndrome
hypothyroidism
medications that increase triglycerides](https://image.slidesharecdn.com/dyslipidemiapresentation-231007141849-8eed9ada/75/Dyslipidemia-presentation-pptx-32-2048.jpg)
![In adults with severe hypertriglyceridemia (fasting
triglycerides ‡500 mg/dL [‡5.7 mmol/L], and espe- cially
fasting triglycerides ‡1000 mg/dL [11.3 mmol/L]), it is
reasonable
To look and treat reversible causes
Consider statin in maximum doses
Fibrate drugs](https://image.slidesharecdn.com/dyslipidemiapresentation-231007141849-8eed9ada/75/Dyslipidemia-presentation-pptx-33-2048.jpg)























![4. In patients with severe primary
hypercholesterolemia (LDL-C level ‡190
mg/dl[‡4.9 mmol/L]), without calculating 10-year
ASCVD risk, begin high-intensity statin therapy.](https://image.slidesharecdn.com/dyslipidemiapresentation-231007141849-8eed9ada/75/Dyslipidemia-presentation-pptx-57-2048.jpg)



