Based on the limited information provided:
- Diagnosis: Thrombotic thrombocytopenic purpura (TTP)
- Management: Plasma exchange to remove ADAMTS13 inhibitor
More information is needed to confirm the diagnosis and guide appropriate treatment. Some key questions include:
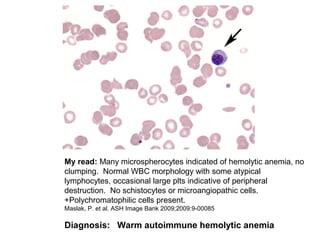
- Is there evidence of schistocytes on the peripheral smear?
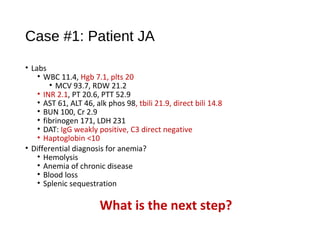
- What is the patient's coagulation profile and haptoglobin level?
- Is ADAMTS13 activity level reduced?
- What is the patient's medical history and any potential triggers?
- Are there any neurologic deficits on exam beyond altered mental status?
Without confirming the presence of schistocytes and reduced ADAMTS13