The new FAST CARE software from Siemens aims to standardize and simplify CT scans through several innovations. It guides users intuitively through the entire scan process from planning to reconstruction. This reduces workload and potential for errors. FAST CARE also facilitates dose reduction through tools like iterative reconstruction and automatic selection of optimal scan parameters. Dr. Michael Lell expects FAST CARE to save time and improve efficiency, allowing clinics to examine more patients with fewer resources. He is also hopeful the automatic coupling of contrast injection and scanning can reduce staffing needs. Overall, FAST CARE makes CT scans safer, more reproducible and effective for both patients and clinicians.













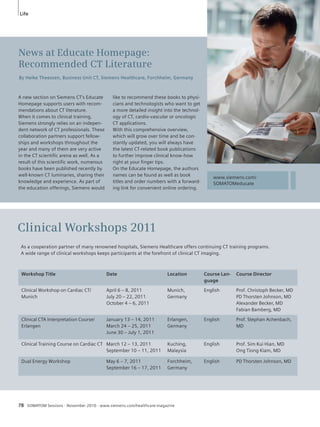
![Topic
1 80-year old patient with severe aortic valve stenosis prior to trans-catheter
aortic valve implantation (TAVI). Pre-procedural Flash Spiral
angiography was performed using high-pitch spiral data acquisition pro-spectively
triggered at 60% of the R-R interval (128 x 0.6 mm slices,
100 kV, 320 mAs, SOMATOM Definition Flash). For thoraco-abdominal
angiography including the coronary arteries (Arrowhead) only 40 ml of
contrast agent was used (flow rate 4 ml /s). Estimated effective radiation
dose was 4.3 mSv. at a scan time of 1.7 seconds.
Images show assessment of aortic annulus diameters in syngo.via (Fig.
1A dotted line) as well as distances between the aortic annulus and the
coronary ostia. In addition, peripheral arteries have been evaluated for
significant stenosis (Fig. 1B). The red arrow indicates an occluded iliac
artery, making transfemoral access impossible here. The same data also
shows pronounced calcification along the whole thoracic aorta (Fig. 1C).
1 Cardiovascular News, Transcatheter heart valve
replacement: A European perspective,
www.cxvascular.com, Jan 2010
2 Valve Implantation for Aortic Stenosis in Patients
Who Cannot Undergo Surgery, N Engl J Med
2010
3 Aregger F, Wenaweser P, Hellige GJ, et al. Risk of
acute kidney injury in patients with severe aortic
valve stenosis undergoing transcatheter valve
replacement. Nephrol Dial Transplant 2009; 24:
2175–2179.
4 Vahanian A, Alfieri OR, Al-Attar N, et al. Transcath-eter
valve implantation for patients with aortic
stenosis: a position statement from the European
Association of Cardio-Thoracic Surgery (EACTS)
and the European Society of Cardiology (ESC), in
collaboration with the European Association of
Percutaneous Cardiovascular Interventions
(EAPCI). EuroIntervention 2008; 4: 193-199.
2 Up to 60%
less contrast
media by use of
high-pitch spiral
DSCT angio-graphy
of the
complete aorta
– compared to
other CT tech-nologies.
Courtesy of
University
of Erlangen-
Nuremberg,
Erlangen,
Germany
140 ml*
100 ml#
SOMATOM Sessions · November 2010 · www.siemens.com/healthcare-magazine 17
gies need about 6–9 seconds). This per-mits
a tremendous reduction of contrast
agent by 50–60%, which is crucial for
patients with renal insufficiency under-going
a subsequent TAVI procedure.
Compared to approximately 100–140 ml
of contrast agent needed in the past for
a CT angiography of the entire aorta, it
is now possible to use only 40 ml (flow
rate 4 ml/s) for the same examination,
which poses a significantly reduced risk
of Contrast Induced Nephropathy (CIN)
in this patient population (Fig. 2).
Accurate and fast planning
with syngo.via
The decision whether a patient is suit-able
for a catheter-based procedure and
the pre-operative planning with the
selection of the access route are based
upon results of the CT angiography. The
size of the aortic annulus for selection of
the valve prosthesis and the angulation
of the invasive fluoroscopy which allows
for simulating the optimal projection of
the aortic valve during the TAVI proce-dure
can be predicted from the same
DSCT angiography data with the support
of syngo.via.* This leads to further con-trast
media savings during the invasive
procedure since the syngo.via* software
automatically provides the correspond-ing
C-arm position.
On the basis of this protocol and ana-tomical
measurements by Flash Spiral
CT, physicians are able to quickly per-form
more patient friendly and precise
catheter-based procedures.
The time consuming planning of the
procedure is very well supported by the
many automated pre-processing steps
in the new syngo.via* software which
in early tests could show to reduce plan-ning
time by more than 33% (10 min.
versus 15 min.).
In a nutshell: Flash Spiral
and syngo.via
In conclusion the Definition Flash,
combined with the highly automated
syngo.via* workflow modules, provide
the most possible patient friendly and
accurate pre-operation planning solution
available. The high potential for cost
reduction coming from fewer patients
suffering acute CIN and therefore
requesting less of the expensive aftercare
is not yet taken into account herein.
SOMATOM Definition Flash:
www.siemens.com/SOMATOM-Definition-
Flash
CT Cardiovascular Engine:
www.siemens.com/CT-cardiology
Single-Source CT
for Abdominal
Aorta
160
140
120
100
80
60
40
20
0
*Loewe C, Eur Radiol 2010; #Wu W, AJR 2009; §Flash Thorax Protocol
40 ml§
Amount of Contrast Agent [mL]
Single-Source CT
for Triple Rule Out
Dual Source CT
SOMATOM
Definition Flash
2
News
* syngo.via can be used as a standalone device or
together with a variety of syngo.via based soft-ware
options, which are medical devices in their
own rights.
1C](https://image.slidesharecdn.com/somatomsession27-00079186-00270172-140821163309-phpapp01/85/Somatom-session-27-17-320.jpg)









![Business
Right after its introduction, the manufacturing lines of the SOMATOM Definition AS
were filled and have remained filled since then.
SOMATOM Sessions · November 2010 · www.siemens.com/healthcare-magazine 31
With the introduction of the SOMATOM
Definition AS – the world’s first Adaptive
Scanner – in 2007, Siemens opened
a new chapter in single-source CT tech-nology.
The revolutionary idea was to
combine high-end CT imaging for any
clinical task at lowest possible dose with
a scanner design that didn’t exclude
patients because of the system’s geome-try.
And all this with a footprint small
enough to fit it into literally minimum
space. The result: for the first time, a
system actively adapts itself to virtually
every clinical situation. Offering a 128-
slice CT system with a pitch-independent
isotropic resolution of 0.33 mm, a rota-tion
time of 0.3 seconds and 100 kW
generator power, it delivers enough
reserves to meet virtually all clinical
tasks. With a 78 cm bore diameter, a scan
range of 200 cm that can be acquired in
approximate 10 seconds at highest reso-lution
and a table load capacity of up to
300 kg, whole body examinations in
acute care or bariatric imaging were
turned into clinical routine. Groundbreak-ing
innovations introduced new dimen-sions
in CT: the Adaptive 4D Spiral over-came
the limitations of a static detector
design and allowed covering whole
organs in 4D – and the still unique 3D
interventional suite provided 3D guided
intervention support. This was all realized
within a system that could be fit nearly
everywhere with only an 18 m² footprint,
freely selectable air or water cooling and
full on-site upgradeability.
After the first installations, users were
immediately excited. Among the first was
Prof. Joe Schoepf from the Medical Uni-versity
of South Carolina. In an interview,
he commented that the “Definition AS
will effectively overcome a number of
limitations we face today. […] All the
guess work is taken out” and it “has all
the power […] to capture clear images
unmarred by excess noise, even in obese
patients.” Following this excitement,
many publications proved that the
SOMATOM Definition AS kept the prom-ises
given. In 2009, a new software ver-sion
was rolled out to all customers,
underlining Siemens’ dedication to cus-tomer
care. With innovative features like
Neuro BestContrast, it boosted the
already outstanding image quality even
further and made IRIS – the Iterative
Reconstruction in Image Space – avail-able
for the SOMATOM Definition AS.
Naturally, this convinced the market and
the result was the fastest ramp-up in
Siemens CT’s history. After the first
installation in May 2008, the SOMATOM
Definition AS surpassed 500 installations,
in September 2009, and then achieved
the 1,000th installation in September
2010 in Washington DC, USA.
Now, Siemens has taken the SOMATOM
Definition AS to the next level with the
introduction of FAST CARE at this year’s
RSNA. For decades, Siemens has spear-headed
dose reduction and has intro-duced
many innovations following the
“As Low as Reasonably Achievable”
(ALARA) principle. For this, Siemens’ initi-ated
its CARE (Combined Applications to
Reduce Exposure) philosophy more than
15 years ago. Additionally, the SOMATOM
Definition AS brought many innovations
like the Adaptive Dose Shield that, for the
first time, virtually eliminated unneces-sary
over-radiation in every spiral scan.
The new FAST (Fully Assisting Scanner
Technologies) philosophy now aims to
give customers the possibility to maxi-mize
clinical outcome – meaning to
achieve best clinical results, but with
significantly less resources bound to the
CT system. The ultimate goal: provide
medical professionals more time for
patients – or patient-centric productivity.
The new FAST features, like FAST Plan-ning
or FAST Spine, simplify typically time
consuming and complex procedures. The
scanning process gets more structured
and results become more reproducible.
Integrating the capabilities of syngo.via,*
Siemens’ revolutionary, new imaging
software, the complete examination –
from scan preparation to data evaluation
– is streamlined. This gives medical pro-fessionals
significantly more time for
what is of utmost importance: the diag-nosis
and interaction with their patients,
leading ultimately to improved clinical
results with less patient burden. This
combination of highest image quality at
lowest dose and highest patient-centric
productivity is the lever to maximizing
clinical outcomes. The new SOMATOM
Definition AS with FAST CARE will be
available from March 2011.
* syngo.via can be used as a standalone device or
together with a variety of syngo.via based soft-ware
options, which are medical devices in their
own rights.](https://image.slidesharecdn.com/somatomsession27-00079186-00270172-140821163309-phpapp01/85/Somatom-session-27-31-320.jpg)








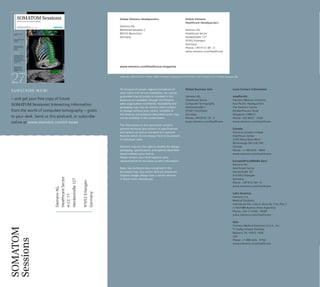
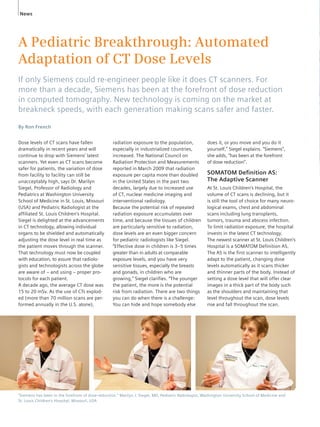
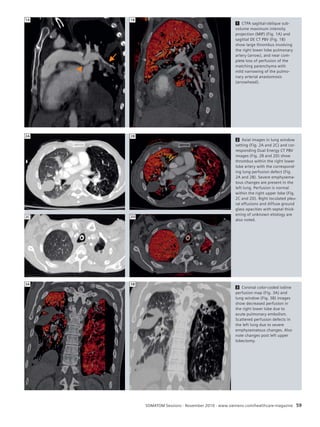
![Clinical Results Cardio-Vascular
Case 3
CT Dynamic Myocardial Stress Perfusion
Imaging – Correlation with SPECT
Kheng-Thye Ho, FACC,* Kia-Chong Chua, MSC,*
Ernst Klotz,** and Christoph Panknin,**
*Department of Cardiology, Tan Tock Seng Hospital, Singapore, Republic of Singapore
**Business Unit CT, Siemens Healthcare, Forchheim, Germany
HISTORY
A 61-year-old male with cardiac risk fac-tors
of hypertension and hyerlipidemia
presented with symptoms of atypical
chest pain. Resting ECG was unremark-able.
Dipyridamole-stress nuclear myocar-dial
perfusion imaging (NMPI) had dem-onstrated
a very large, reversible defect
involving the apex, anterior wall and sep-tum.
The total defect size was quantified
1
42 SOMATOM Sessions · November 2010 · www.siemens.com/healthcare-magazine
1 CT dynamic stress MPI with SPECT
correlation in the mid-ventricular short
axis (1A) and the horizontal long axis
view (1B). Stress are images in the
upper quadrants, rest images below;
CT perfusion to the left of the corre-sponding
SPECT.
2 Invasive angiography findings:
Total occlusion of the proximal LAD
and a 90% lesion in OM3 (2A, arrow),
and 75% lesion in the RPDA branch
of the otherwise normal RCA (2B,
arrowhead).
as 34% of the left ventricle. Left ventricu-lar
ejection fraction was estimated as
65% in the post-stress images by gating.
Post-stress dilatation was noted in the
scan, which is an adverse prognostic sign
in the presence of coronary artery dis-ease.
Invasive coronary angiography
demonstrated total occlusion of the prox-imal
LAD, with collaterals arising from
both the LCx and RCA. There was also a
90% lesion in the third obtuse marginal
branch (OM3) and a 75% lesion in the
right posterior descending artery (RPDA)
branch of the right coronary artery
(RCA). CT myocardial perfusion imaging
(MPI) was performed prior to CABG.[1]
The patient underwent successful coro-nary
bypass surgery, with a left internal
1A 1B
2A 2B](https://image.slidesharecdn.com/somatomsession27-00079186-00270172-140821163309-phpapp01/85/Somatom-session-27-42-320.jpg)

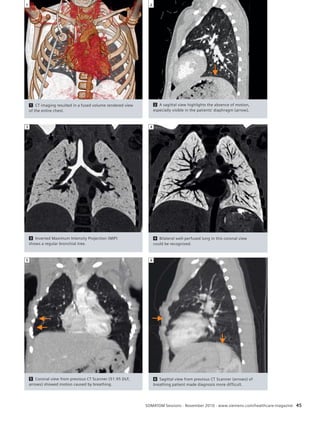
![Case 4
SOMATOM Defi nition Flash
Motion-free Thoracic Infant Scan: Follow-Up
Study After Chemotherapy
By Susann Skoog, MD, Nils Dahlström MD, and Petter Quick
Department of Radiology and Center for Medical Image Science and Visualization (CMIV),
Linköping University Hospital, Linköping, Sweden
HISTORY
A three-year-old boy with small
(7-8 mm diameter) lung metastases
from a germ-cell tumor, successfully
treated with chemotherapy, was
referred for follow-up CT of the thorax.
In a previously acquired CT-examination
without sedation, utilizing DLP 51.95
mGycm, 3.28 mGy CTDi vol / scan
length 140 mm, the patient had been
coope rative.
In the present Flash scan, no remaining
metastases were identified and the
serum tumor marker Alpha Fetoprotein
(AFP) levels were normal.
EXAMINATION PROTOCOL
DIAGNOSIS
The ultra-fast thoracic scan mode, using
pitch value of 3, did not reveal any met-astatic
lesions or other pathological find-ings
in the thorax. Both lungs were well
perfused and there was no sign of any
enlarged lymph nodes. The size of the
thymus was increased moderately.
Inverted maximum intensity projection
(MIP) showed a regular bronchial tree.
COMMENTS
Continuous follow-up CT examinations
are necessary to monitor the treatment
effect and determine the complete
Scanner SOMATOM Definition Flash
Scan mode Flash Spiral Thorax Eff. Dose 0.54 mSv
Scan area Thorax CTA Pitch 3
Scan length 172 mm Slice collimation 128 x 0.6 mm
Scan direction Cranio-caudal Slice width 0.75 mm
Scan time 0.42 s Reconstruction increment 0.6 mm
Tube voltage 120 kV Reconstruction kernel B31f
Tube current 20 mAs Contrast
Dose modulation CARE Dose4D Volume 30 ml Ultravist® 370 mg / ml
CTDIvol 1.23 mGy Flow rate 1 ml/s
Rotation time 0.28 s Start delay 30 s
DLP 30 mGy cm Postprocessing syngo InSpace4D
44 SOMATOM Sessions · November 2010 · www.siemens.com/healthcare-magazine
patient response. Using the high-pitch
spiral acquisition of the SOMATOM
Definition Flash CT, patients can always
be examined with greatly reduced radia-tion
dose in comparison to standard CT
protocols. In this case only 0.54 mSv*
were necessary to be applied.
The fast scan mode which acquired the
patients’ thorax in only 0.42 seconds
avoided the need to sedate this pediatric
patient. The resulting images were
obtained motion free and delivered excel-lent
and valuable data for a safe diagno-sis
without the need of a second scan.
Clinical Results Oncology
* Effective Dose was calculated using the published conversion factor for a pediatric (5 year old) chest of 0.036 mSv (mGy cm)-1 [1].
To take into account that Siemens calculates the CTDi in a 32 cm CTDi phantom, an additional correction factor of 2 had to be applied.
[1] McCollough CH et al Strategies for Reducing Radiation Dose in CT.](https://image.slidesharecdn.com/somatomsession27-00079186-00270172-140821163309-phpapp01/85/Somatom-session-27-44-320.jpg)



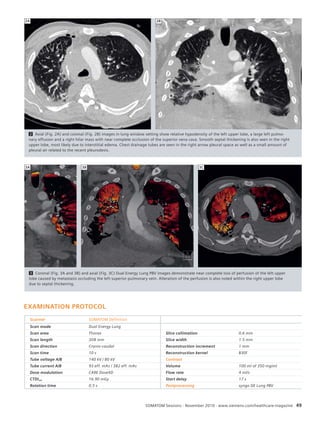
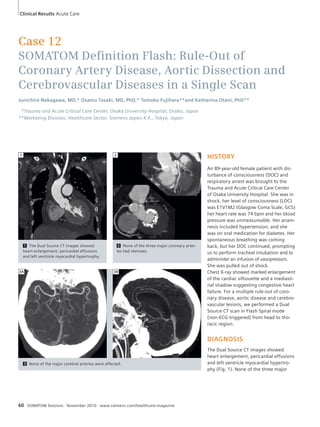
![Case 7
SOMATOM Spirit: Follow-Up Examination
of Cerebral Meningioma
By Wolfgang Gerlach, MD,* Andreas Blaha**
*Private Practice, Heidenheim, Germany,
**Business Unit CT, Siemens Healthcare, Forchheim, Germany
HISTORY
This 74-year-old female patient under-went
a regular follow up procedure
of the known meningioma located
in the ventral part of the clivus. To
exclude progress of the meningioma
a CT-Angiography was ordered.
DIAGNOSIS
The cerebral CT-Angiography (CTA) was
performed with 80 ml of contrast media
to achieve a good delineation of the
meningioma. A homogeneous opacifica-tion
of the lesion needed to be achieved
(Mean density could be measured with
110 Hounsfield units, HU). The menin-gioma
is situated at the clivus, almost
extending to the foramen magnum. The
size was measured with 2.9 x 2.5 cm.
The sagittal view of the CTA shows the
extension towards the spinal cord, but no
derogation of the spinal cord could be
seen. No abnormity of the cerebral vas-cular
system could be detected.
COMMENTS
The patient requires continuous moni-toring
to detect early signs of progression
of the lesion. Therefore a low dose pro-tocol
was selected 0.5 mSv*. No pro-gression
could be observed, so the next
monitoring examination is recommended
in 12 months.
To achieve the pure arterial contrast
1 Cranio-caudal view of the CTA, good opacification of the meningioma (arrow).
1
50 SOMATOM Sessions · November 2010 · www.siemens.com/healthcare-magazine
region of the patients meningioma and
makes it the preferred visualization
method for detecting and monitoring
cerebral meningioma.
timing an automatic contrast bolus
tracking software (CARE Bolus CT) was
utilized. CT provides the exact measure-ment
and location in the very dense
Clinical Results Oncology
* Effective Dose was calculated using the pub-lished
conversion factor for an adult head of
0.0021mSv (mGy cm)-1 [1].
[1] McCollough CH et al. Strategies for Reduc-ing
Radation Does in CT, Radiol. Clin. N. Am. 47:
(2009) 27-40.](https://image.slidesharecdn.com/somatomsession27-00079186-00270172-140821163309-phpapp01/85/Somatom-session-27-50-320.jpg)


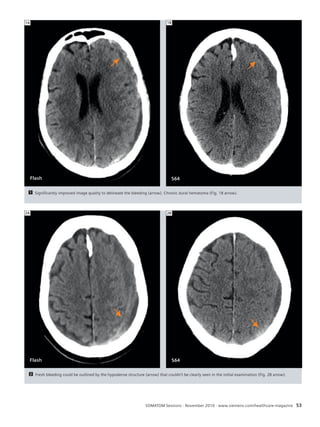










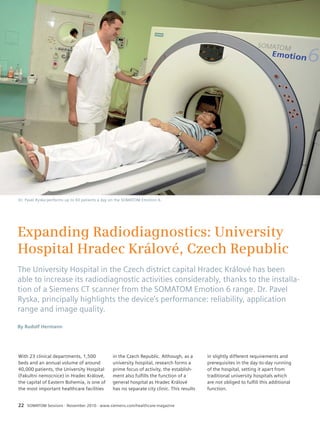
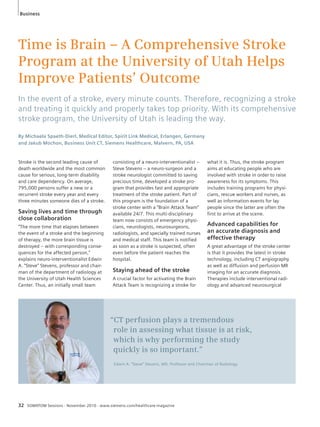
![Science
Dose Parameters and Advanced Dose
Management on SOMATOM Scanners
The measurement and calculation of radiation dose in CT is an important
topic for an effi cient dose management. Quantities such as the CTDI, DLP
and effective dose are useful when used appropriately. Now Siemens takes
dose management to a new level by providing tools such as Dose Structured
Reports and CARE Analytics.
By Stefan Ulzheimer, PhD, Christianne Leidecker, PhD, and Heidrun Endt
Business Unit CT, Siemens Healthcare, Forchheim, Germany
The assessment and management of
patient dose has become one of the most
frequently discussed topics in Computed
Tomography. On SOMATOM Scanners,
the reporting of established dose para-meters
like Computed Tomography Dose
Index (CTDI) and Dose Length Product
(DLP) has been implemented since 1999.
For each exam, the information is avail-able
in the patient protocol, and can be
viewed and archived as a DICOM image.
With Dose Structured Reports (Dose SR)
Siemens is taking the next step to enable
more transparency in terms of radiation
dose. Furthermore, tools like CARE
Analytics provide an easy means to eval-uate
Dose SR.
Technical dose parameters –
CTDIvol and DLP
The CTDI is the primary dose measure-ment
concept in CT and is defined by
the International Electrotechnical Com-mission
(IEC) [1] and adopted by various
national bodies such as for example by
the US Food and Drug Administration
(FDA). The weighted volume CT Dose
Index, CTDIvol represents the average
Calculating effective dose from scanner dose information.
68 SOMATOM Sessions · November 2010 · www.siemens.com/healthcare-magazine
absorbed dose within the scan volume
for standardized phantoms. Their diame-ters
are 16 and 32 cm, to approximate
conditions for head and body examina-tions
so the phantoms do not adequately
represent patient cross-sections. How-ever
the CTDIvol is an objective technical
dose parameter based on a directly mea-sured
quantity. It takes into account pro-tocol-
specific parameters and is useful to
compare different scan protocols across
various CT scanners. Thus, IEC standards
require the prospective display of the
CTDIvol on the console of the CT scanner.
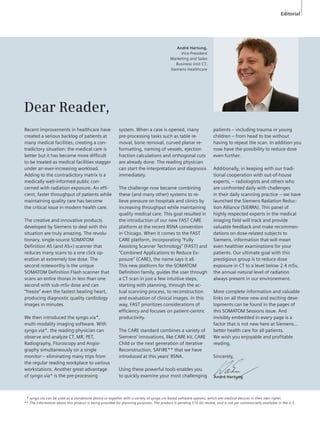
1 Calculating effective
dose for adults. From the
Patient Protocol of this
abdominal scan, the DLP is
obtained:
DLP = 274 mGy·cm
Using the conversion factor
for abdominal exams,
0.015 mSv/(mGy·cm) [3],
effective dose E is estimated
to be E = 274 mGy·cm ·
0.015 mSv/(mGy·cm) =
4.1 mSv
1](https://image.slidesharecdn.com/somatomsession27-00079186-00270172-140821163309-phpapp01/85/Somatom-session-27-68-320.jpg)
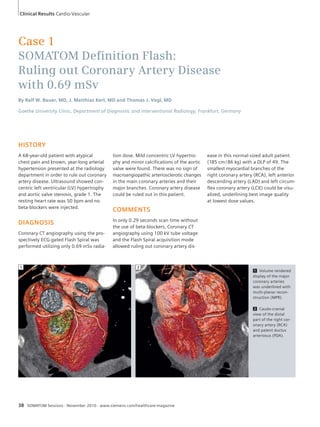
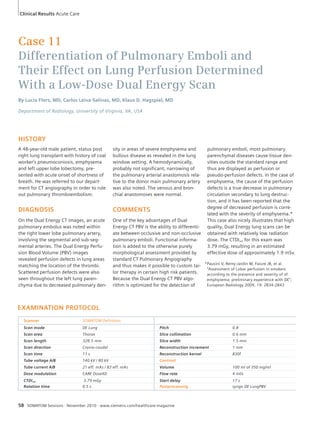
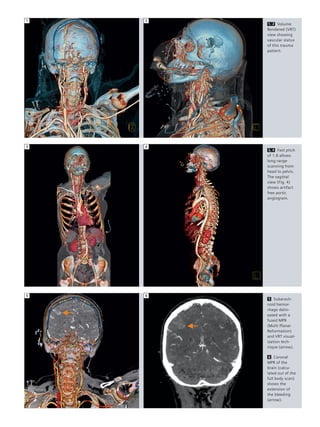
![Science
Calculating effective dose from scanner dose information for a pediatric body exam.
2 Calculating effective dose for children. Using the same values as in the first example, the DLP is: DLP = 274 mGy·cm. First you have to
determine if the DLP refers to a 32 cm or 16 cm CTDI phantom. In this case, the DLP is reported in the 32 cm body CT dose phantom. This value
has to be converted to the head CT dose phantom if pediatric conversion factors published in [table 1] shall be used to compute the effective
dose: DLP = 2.0 * 274 mGy·cm = 548 mGy·cm. Note: Typical values are between 2.0 and 2.4 for Siemens scanners. Values can be found in the
System Owner Manual. Since the method of using conversion factors to determine the effective dose is a very rough method usually using a cor-rection
factor of 2.0 is sufficiently accurate for all scanners. For a 5-year old child, a factor of 0.02 mSv/(mGy·cm) for abdominal exams is used
[table 1] to estimate E. E = 548 mGy·cm · 0.02 mSv/(mGy·cm). = 11 mSv. If the DLP was already measured in the 16 cm head phantom like it is
the case on new scanners the conversion factors from table 1 can be used directly without applying an additional factor of 2.0 to 2.4.
SOMATOM Sessions · November 2010 · www.siemens.com/healthcare-magazine 69
To represent the overall dose of a given
scan protocol, the CTDIvol is multiplied
with the examination range which then
yields the DLP.
Towards assessing
patient dose
When asking the question of “what is
the radiation dose”, one really is inter-ested
in “what is the risk of this exam”?
However, information on individual
patient dose depends on multiple para-meters,
such as patient specific character-istics
and in addition to the technical
parameters of the system and exam.
The International Commission on Radia-tion
Protection (ICRP) has introduced the
concept of effective dose which repre-sents
a risk-related quantity for the con-trol
of radiation exposure and optimiza-tion
of protection. It cannot be measured
directly, but rather is calculated using
defined dosimetric models. Hence, it
applies to a reference person and does not
provide risk information for the individual.
Table 1
Region of body Conversion factor from DLP to Effective Dose in [mSv / (mGy ·cm)]
0 year old 1 year old 5 year old 10 year old Adult
Head and neck 0.013 0.0085 0.0057 0.0042 0.0031
Head 0.011 0.0067 0.0040 0.0032 0.0021
Neck 0.017 0.012 0.011 0.0079 0.0059
Chest 0.039 0.026 0.018 0.013 0.014
Abdomen and pelvis 0.049 0.030 0.020 0.015 0.015
Trunk 0.044 0.028 0.019 0.014 0.015
One practical method to calcu-late
effective dose: Conversion
factors from DLP to effective
dose for children and adults;
for different body regions as
published in [2, 3]. Please note
that the conversion factors for
children refer to a DLP measured
in a 16 cm phantom. On older
scanners or software versions
the DLP in pediatric protocols
often refers to a 32 cm phantom.
Then an additional correction
factor has to be applied.
2](https://image.slidesharecdn.com/somatomsession27-00079186-00270172-140821163309-phpapp01/85/Somatom-session-27-69-320.jpg)
![Science
3 The Dose SR can
be viewed on the
scanner console,
sent to PACS or to
an independent
server used to mon-itor
dose data.
3
Practical ways to determine
effective dose for CT exams
Several approaches to estimate effective
dose for CT exams have been investi-gated.
A generic method was proposed
to estimate effective dose from the DLP
of an exam [2], with the DLP being
reported on most systems. Conversion
factors for normalized effective dose per
DLP were obtained from Monte Carlo
calculations of effective dose for various
clinical exams. These conversion factors
depend only on the region of the body
being scanned (head, neck, thorax,
abdomen, or pelvis).
It is important to understand that calcu-lating
effective dose using this method
can always only be a rough estimate of
effective dose because many parameters
that influence effective dose are not
taken into account. The body size and
the exact location of the scanned area in
relation to the dose sensitive organs are
only two of those parameters. However,
usually this method is sufficiently exact
for the purpose the effective dose con-cept
was developed for: Radiation protec-tion
and getting an estimate on the total
exposure that is also comparable with
other sources of radiation.
As an example, Figure 1 illustrates the
calculation of the effective dose of an
abdominal scan using conversion factors
published by Shrimpton et al. [table 1].
Special considerations
for children
Conversion factors are also available for
children of various ages [table 1].
Special attention has to be paid to the fact
that the conversion factors published
apply to values reported in the head CT
70 SOMATOM Sessions · November 2010 · www.siemens.com/healthcare-magazine
dose phantom.
In the past scanners, CTDI values were
reported in the head CT dose phantom
for head exams and the body CT dose
phantom for body exams, irrespective of
the patient age. This was in line with the
original IEC standards, which did not
provide instructions for pediatric exams.
Thus, for calculations regarding pediatric
body exams, an additional calculation
step has to be performed, as illustrated
in Figure 2.
The example shown illustrates that the
same exposure leads to an effective dose
that is almost three times higher for a
five year old than an adult. While being
purely theoretical, the example shows
that, it is of utmost importance to pay
special attention when imaging pediatric
patients, in particular to use dedicated
pediatric protocols in combination with](https://image.slidesharecdn.com/somatomsession27-00079186-00270172-140821163309-phpapp01/85/Somatom-session-27-70-320.jpg)
![Science
References
1 IEC 61223-2-6 Evaluation and routine testing in
medical imaging departments – Part 2-6: Con-stancy
tests – Imaging performance of computed
tomography X-ray equipment
2 Jessen KA, Panzer W, Shrimpton PC, et al. EUR
16262: European Guidelines on Quality Criteria
for Computed Tomography. Paper presented at:
Office for Official Publications of the European
Communities; Luxembourg. 2000.
3 Shrimpton PC, Hillier MC, Lewis MA, Dunn M.
National survey of doses from CT in the UK:
2003. Br J Radiol Dec;2006 79(948):968–980.
[PubMed: 17213302]
SOMATOM Sessions · November 2010 · www.siemens.com/healthcare-magazine 71
CARE Dose4D.
To standardize dose reporting for pediat-ric
patients, future editions of IEC stan-dards
will require dose reporting in the
head CT dose phantom for pediatric
exams, irrespective of the body region
imaged. Starting with software version
syngo CT 2011A, Siemens will implement
this new requirement. As a consequence,
the conversion factors [table 1] can be
directly applied also in pediatric proto-cols.
To ease the transition, the CT dose
phantom size was added to the user
interface and it is also reported in the
Dose SR.
A new standard:
Dose Structured Reports
As the first CT manufacturer Siemens
now provides the new Dose SR almost
across its complete CT product portfolio.
The Dose SR contains comprehensive
data for each irradiation event, the accu-mulated
dose and information about the
context of the exposure. The data is pro-vided
in electronic format that can be
sent to any system which receives, stores
or processes dose information, such as
conventional PACS or workstations.
A new tool to evaluate
Dose Structured Reports:
CARE Analytics
The Dose SR can serve as the center
piece of an institution wide dose quality
control. To evaluate and analyze the
information, Siemens provides a new
free tool, CARE Analytics. It is a stand-alone
tool and can be installed on an
office computer.
With CARE Analytics, one can query Dose
SR from DICOM nodes directly. Dose
reporting data can be exported and ana-lyzed
with standard tools, such as Micro-soft
Excel™.
With the prompt implementation of
Dose SR and the new tool CARE Analytics
Siemens provides the customer with all
the information needed for a transpar-ent
dose management.](https://image.slidesharecdn.com/somatomsession27-00079186-00270172-140821163309-phpapp01/85/Somatom-session-27-71-320.jpg)