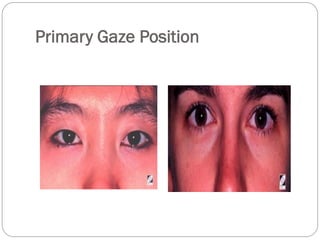
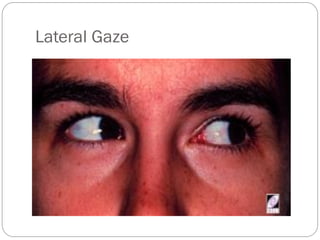
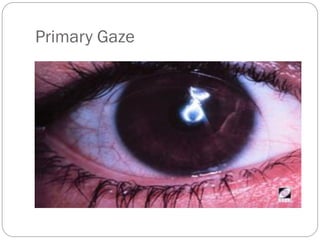
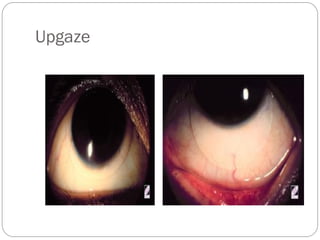
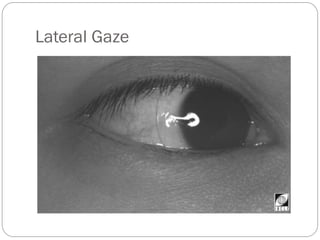
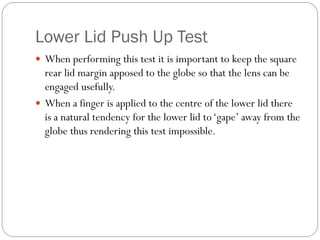
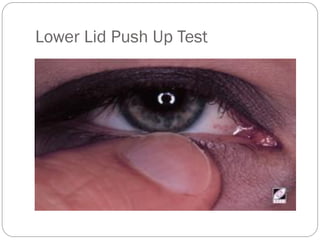
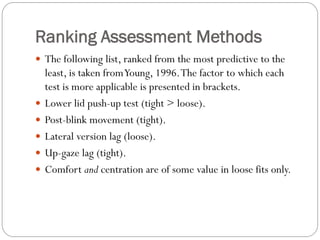
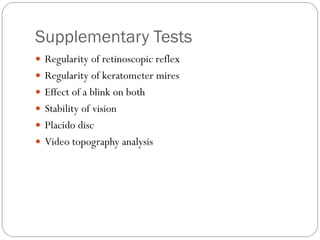
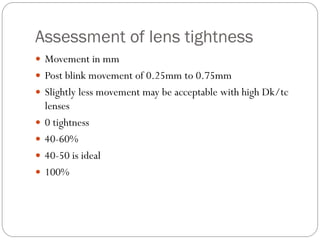
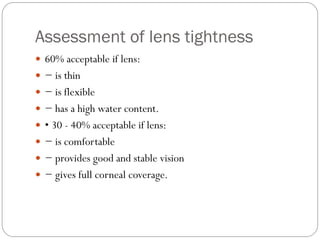
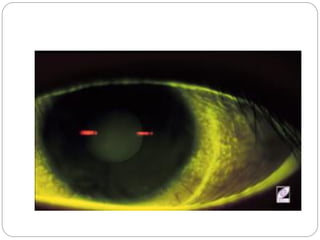
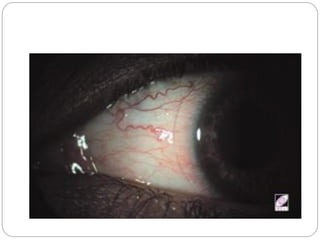
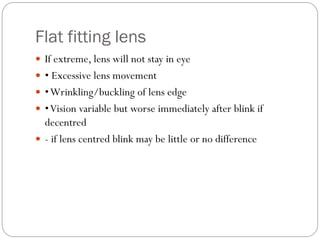
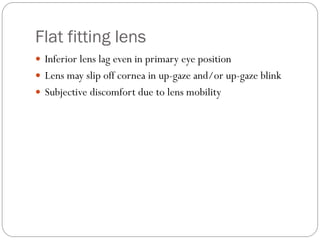
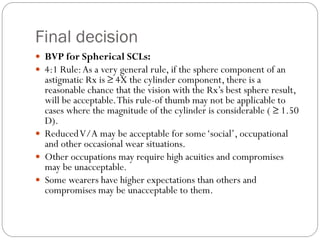
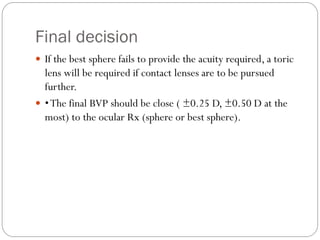
This document discusses guidelines for assessing the fit of trial contact lenses. It recommends assessing lens centration, position, movement, and edge characteristics after 5 minutes and 3-4 hours. Acceptable decentration ranges from 0.2-0.75mm in primary gaze. Lens fit is assessed by observing movement on blink, with lateral gaze, and with lower lid push up tests. Tight fits show little movement while loose fits show more movement or lag. Corneal coverage in all gazes is important. The document provides criteria for acceptable versus unacceptable lens fit characteristics.