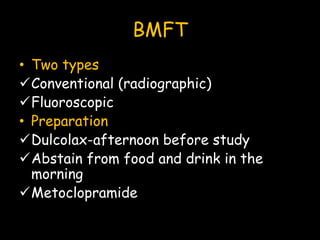
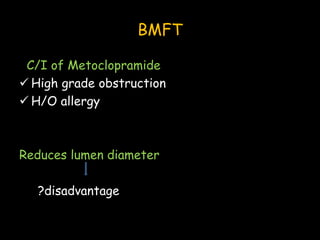
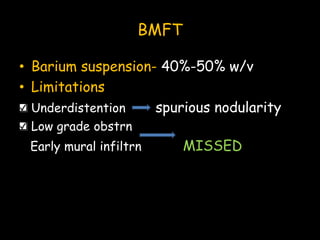
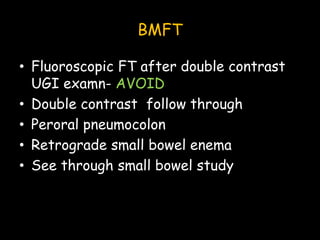
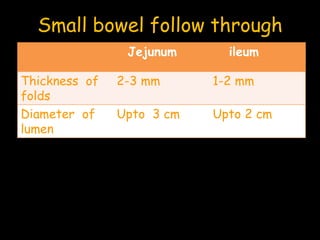
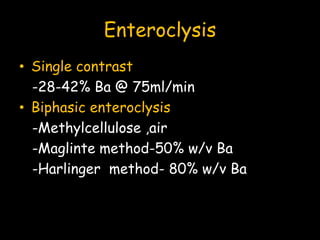
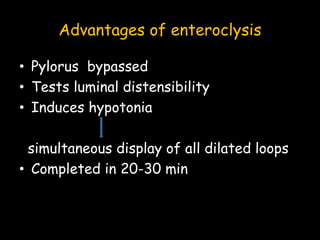
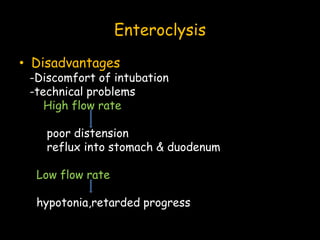
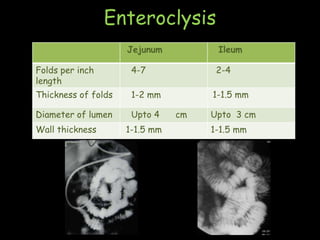
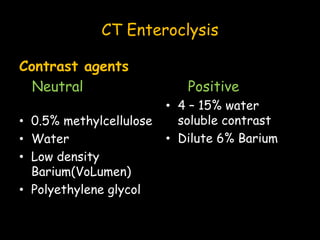
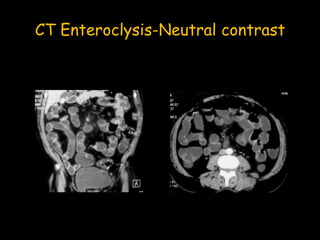
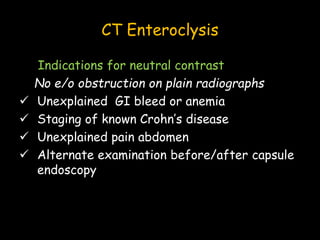
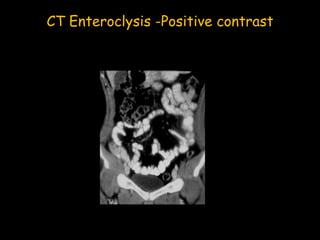
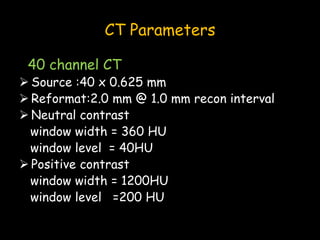
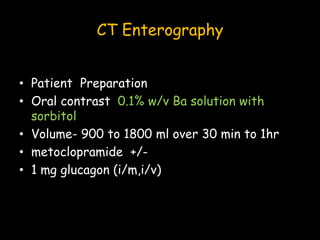
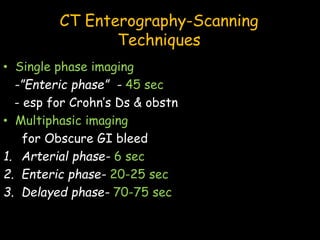
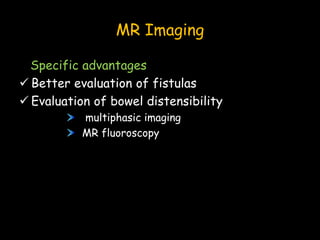
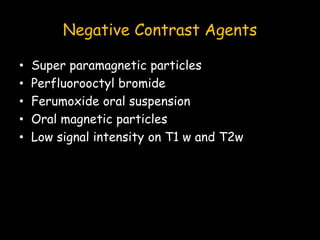
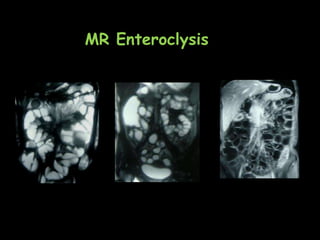
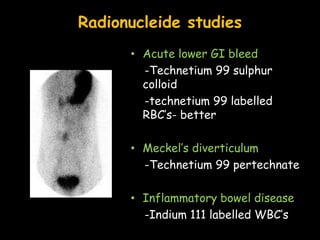
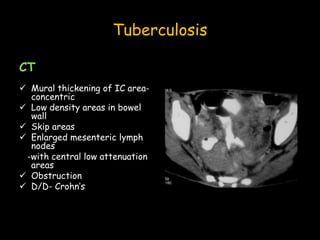
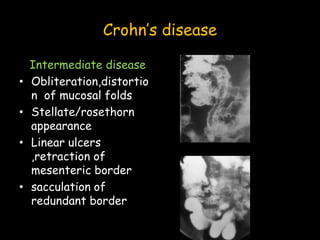
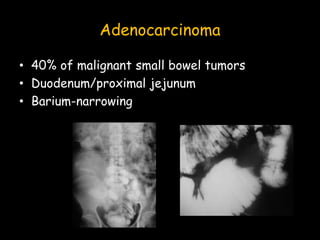
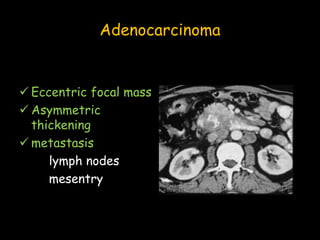
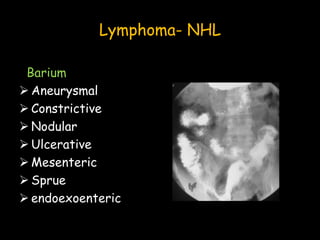
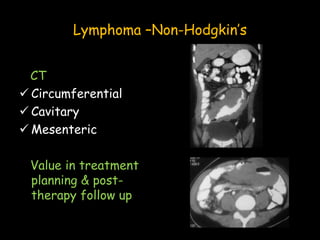
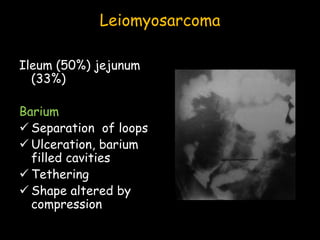
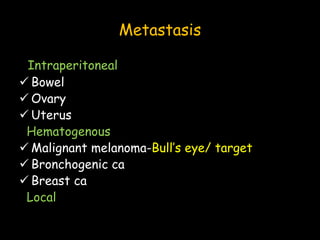
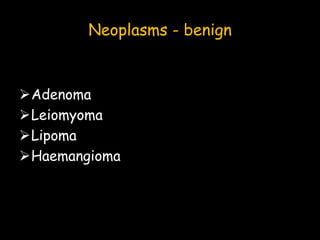
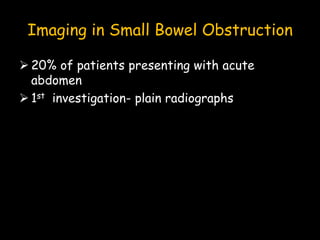
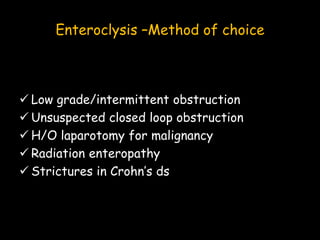
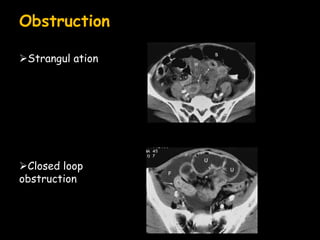
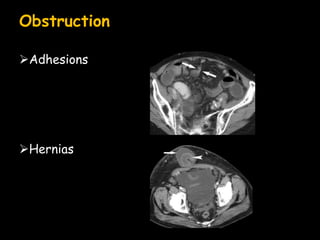
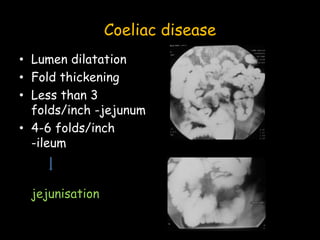
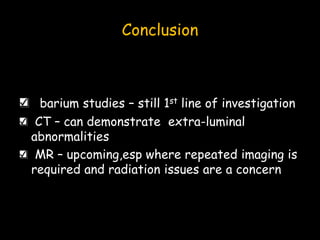
The document presents various imaging modalities for small bowel evaluation, including X-rays, barium studies, CT, MRI, and ultrasound. It discusses the preparation, advantages, and disadvantages of each technique in diagnosing small bowel conditions like inflammatory diseases, neoplasms, and obstructions. Additionally, it outlines the specific applications of CT enteroclysis and MR imaging in detecting and assessing bowel pathology.