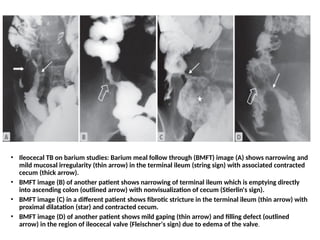
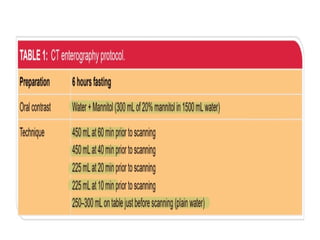
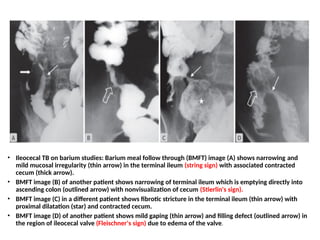
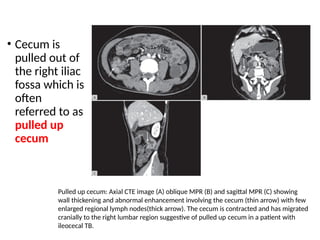
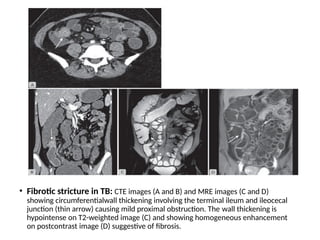
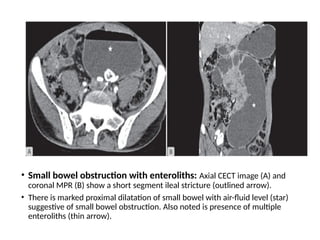
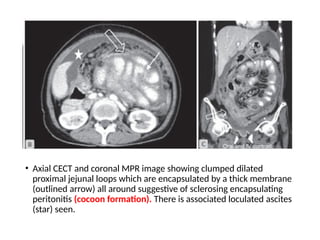
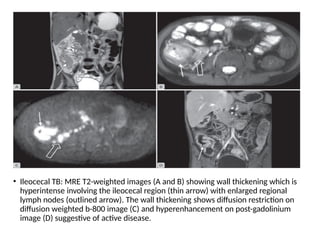
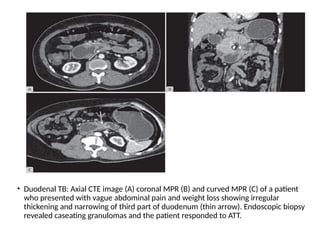
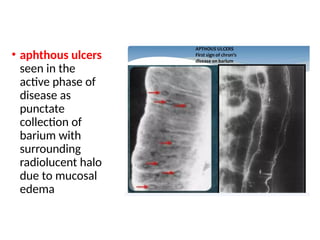
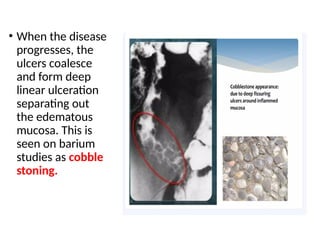
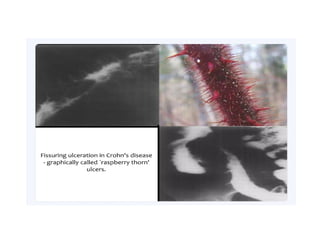
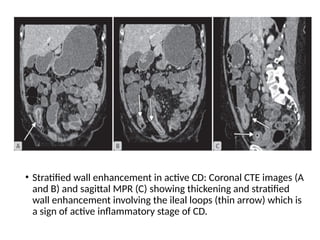
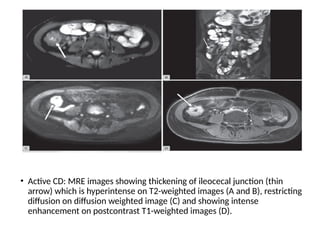
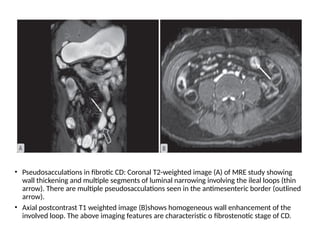
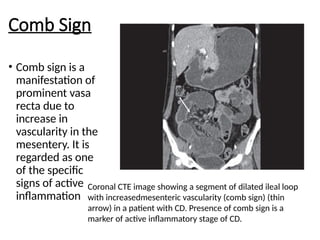
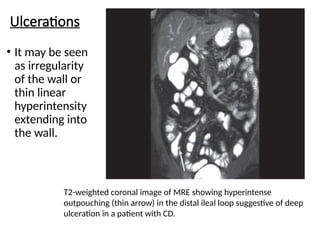
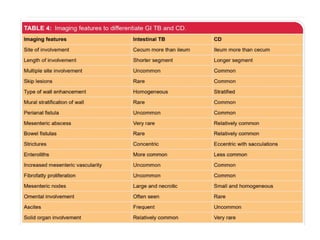
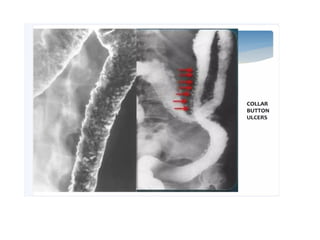
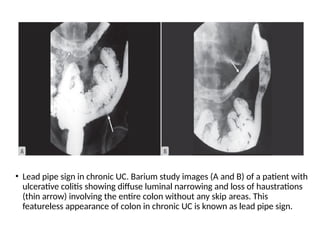
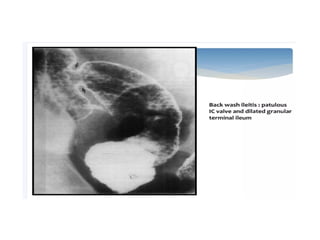
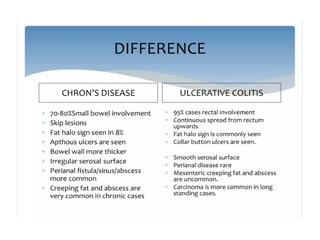
The document discusses advancements in imaging techniques for ulceroconstrictive diseases of the gut, emphasizing the transition from traditional methods like plain radiographs and barium studies to modern approaches such as CT enterography and MRI. It details various imaging modalities' effectiveness in diagnosing gastrointestinal conditions including tuberculosis and inflammatory bowel diseases. Notably, it highlights the diagnostic advantages of newer techniques in assessing bowel strictures and distinguishing between active inflammation and fibrotic changes in conditions like Crohn's disease and ulcerative colitis.