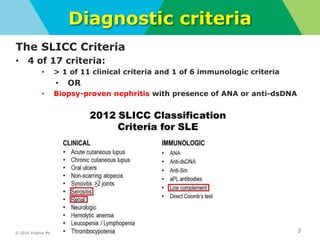
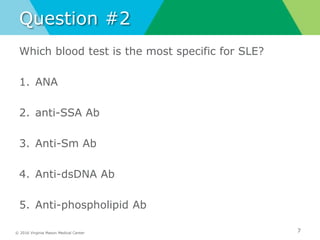
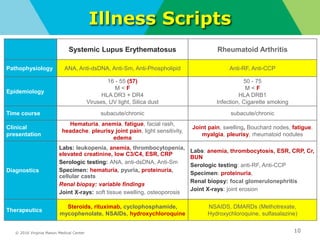
This document summarizes a noon conference presentation on systemic lupus erythematosus (SLE). It reviews the SLICC diagnostic criteria, clinical presentations involving multiple organ systems, laboratory workup including ANA and other autoantibody testing, lupus nephritis, illness scripts comparing SLE to rheumatoid arthritis, and treatment options. The presentation addresses questions about which demographic is most affected by SLE and the most specific blood test for the condition.