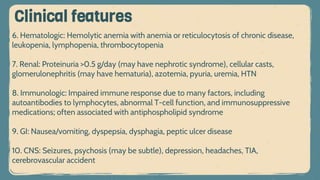
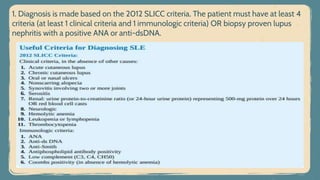
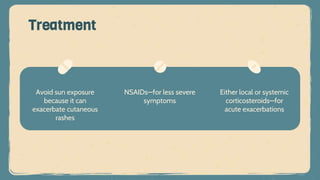
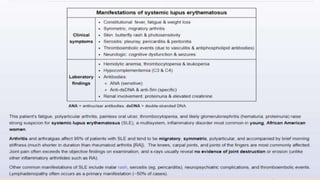
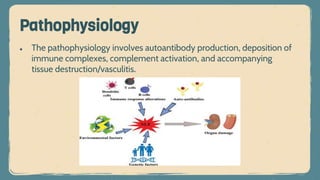
Systemic lupus erythematosus (SLE) is an autoimmune disorder characterized by inflammation and tissue damage across multiple organ systems, influenced by genetic, environmental, and hormonal factors. Diagnosis requires meeting specific clinical and immunologic criteria, typically including positive antinuclear antibodies and various autoantibodies. Treatment focuses on managing symptoms through NSAIDs, corticosteroids, and long-term use of antimalarial agents, with the importance of monitoring for complications such as renal disease.


![3. Musculoskeletal: Arthralgias (may be the first symptom of the disease—found in
90% of patients), arthritis (inflammatory and symmetric, rarely deforming as in
rheumatoid arthritis [RA]), myalgia with or without myositis
Clinical features](https://image.slidesharecdn.com/sle-230328201443-c120e4cc/85/Systemic-lupus-erythematosus-pptx-10-320.jpg)