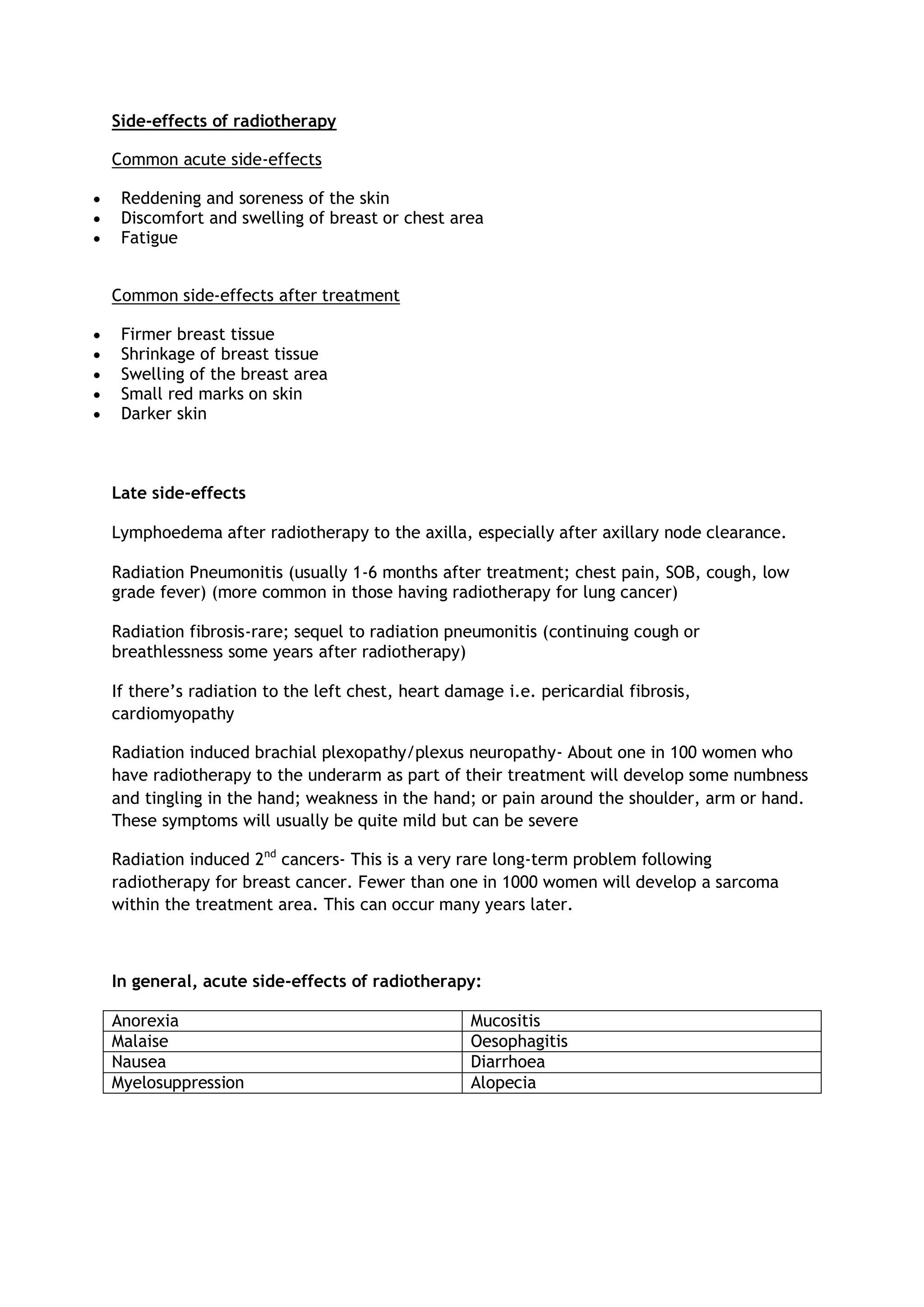
The document discusses potential side effects of radiotherapy. Common acute side effects include reddening and soreness of the skin, discomfort and swelling of the breast area, and fatigue. After treatment, side effects can include firmer or shrunken breast tissue, swelling, and darker skin. Late side effects may include lymphedema, radiation pneumonitis (inflammation of the lungs), and rarely radiation fibrosis (scarring of the lungs) or radiation-induced cancers which occur years later. Radiation pneumonitis specifically occurs in 1-6% of patients and risk increases with use of chemotherapy and a third radiation field. Studies found incidence of interstitial pneumonitis was 8.4 times higher in breast cancer patients than