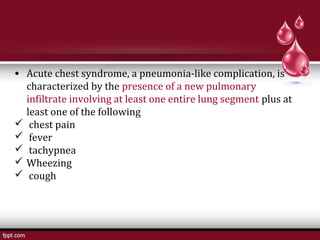
Sickle cell disease is caused by a substitution in the beta globin chain that causes red blood cells to take on a sickle shape in low oxygen conditions. This leads to hemolysis and damage to organs over time. Patients experience painful vasoclusive crises. Management of anesthesia for patients with sickle cell disease requires preoperative correction of anemia, aggressive postoperative pain control to prevent sickling, and watchfulness for acute chest syndrome in the postoperative period. Regional anesthesia techniques are not contraindicated.