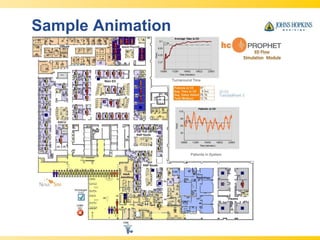
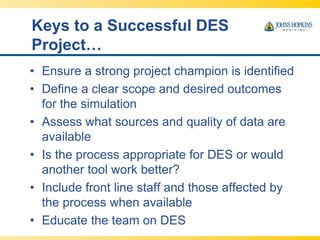
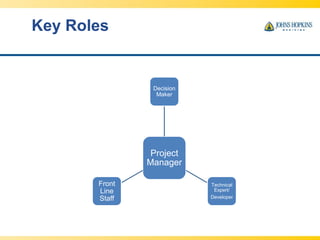
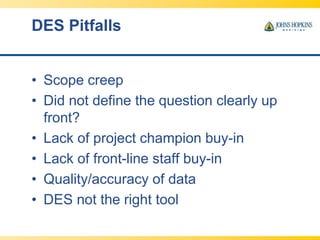
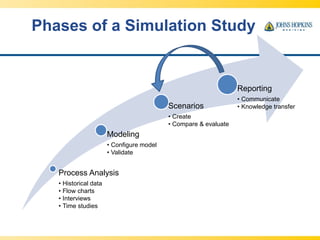
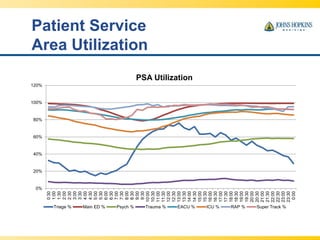
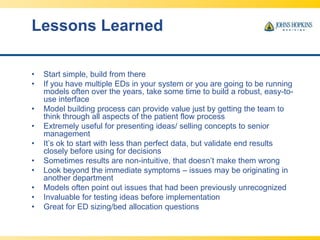
This document discusses using discrete event simulation (DES) to support decision making in emergency departments. DES allows modeling of dynamic patient flow and testing of "what if" scenarios. The document outlines best practices for setting up successful DES projects including defining objectives, gathering quality data, validating models, and including frontline staff. Case studies demonstrate how DES has been used at hospitals to evaluate options for capacity changes, process improvements, and reducing wait times.