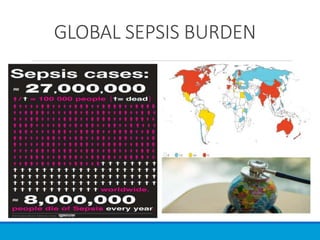
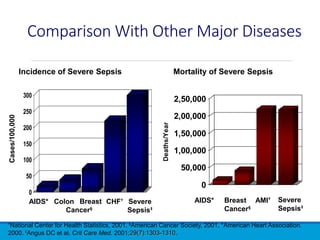
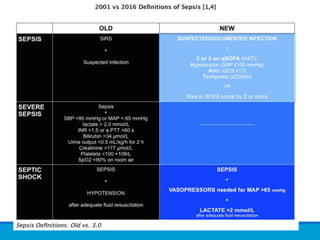
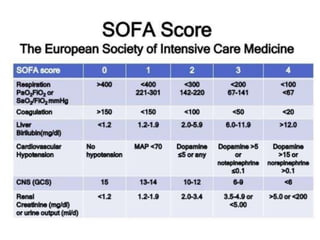
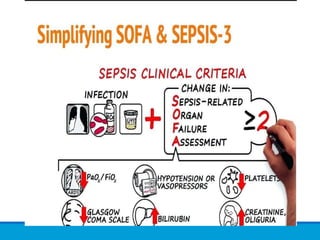
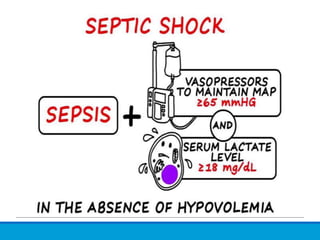
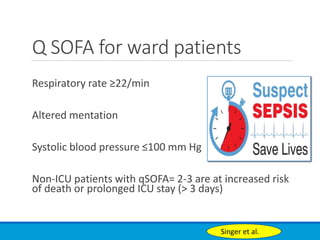
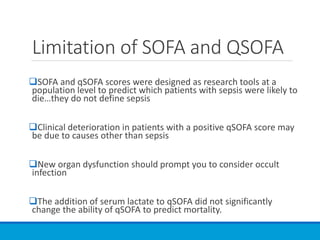
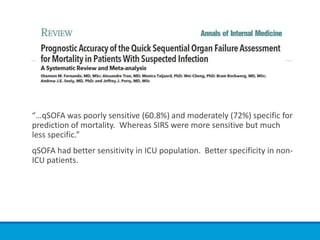
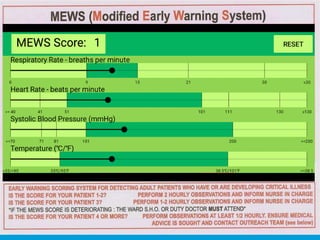
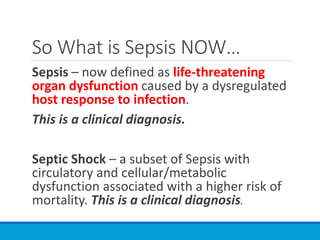
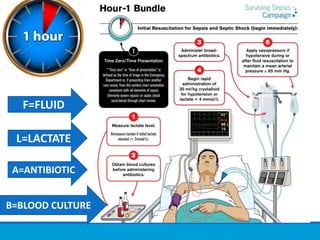
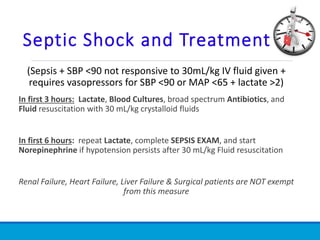
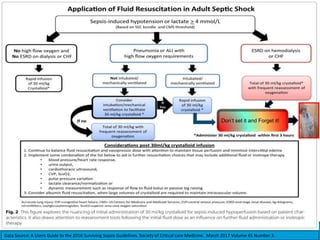
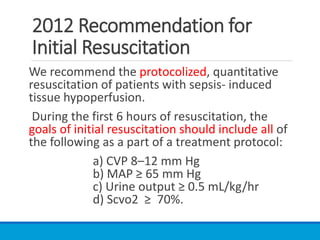
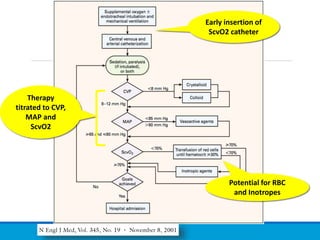
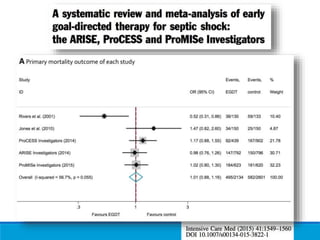
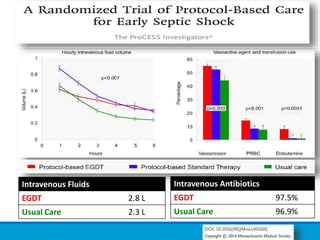
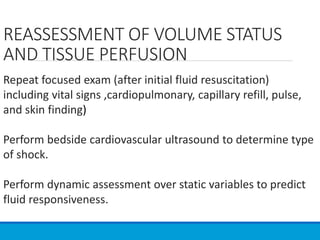
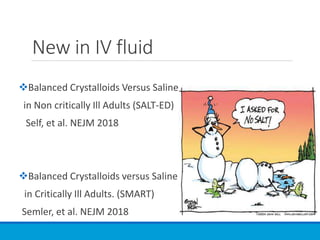
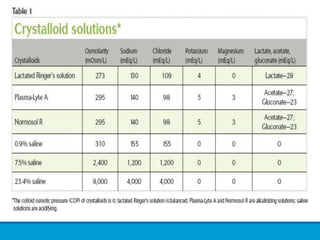
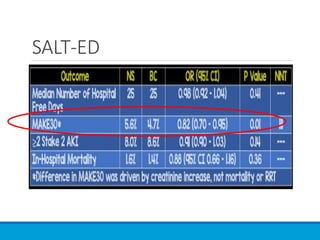
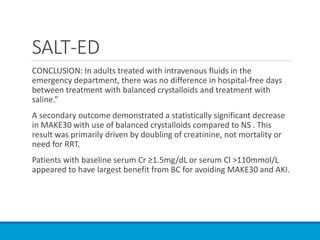
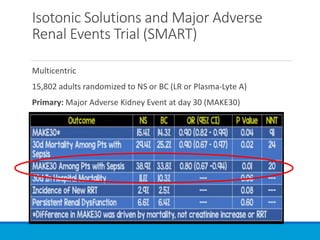
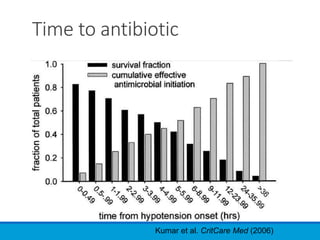
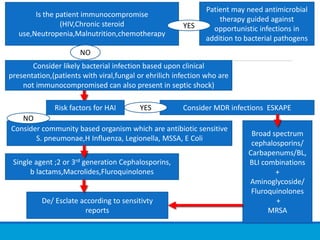
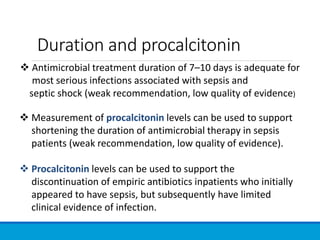
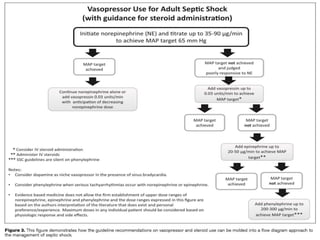
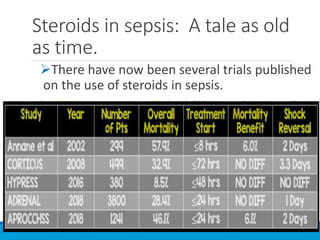
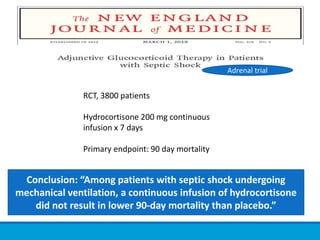
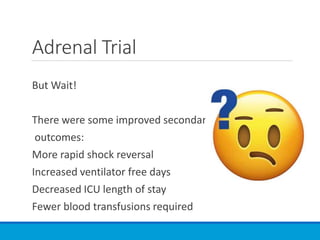
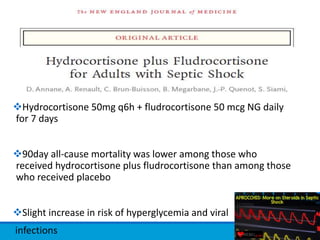
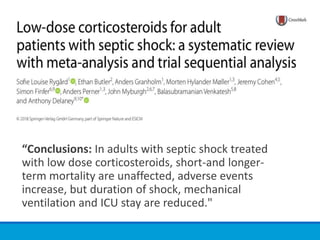
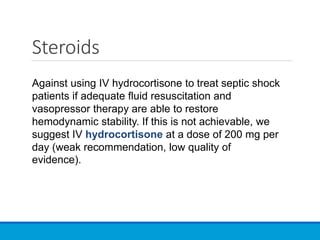
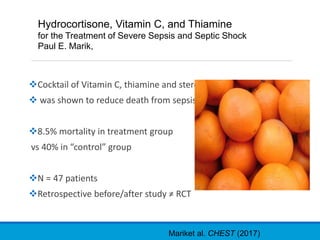
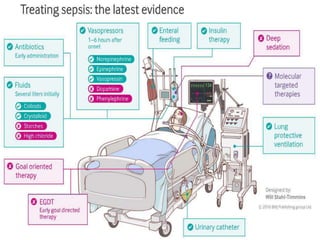
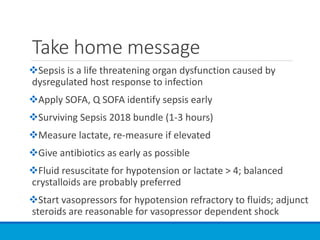
The document discusses recent advancements in the understanding and management of sepsis and septic shock, emphasizing updated definitions, treatment protocols, and the importance of early identification using tools like SOFA and qSOFA scores. It outlines specific resuscitation strategies, including fluid management, the use of antibiotics, and the potential role of adjunct therapies like corticosteroids and vitamin cocktails. The document highlights the necessity for timely intervention to improve patient outcomes and reduce mortality rates associated with these critical conditions.